Here is the google drive link – https://drive.google.com/file/d/1Mc0OOvAct65KCi2WRPT_Jt77Scdk-1oc/view?usp=sharing
Here is the google drive link – https://drive.google.com/file/d/1Mc0OOvAct65KCi2WRPT_Jt77Scdk-1oc/view?usp=sharing
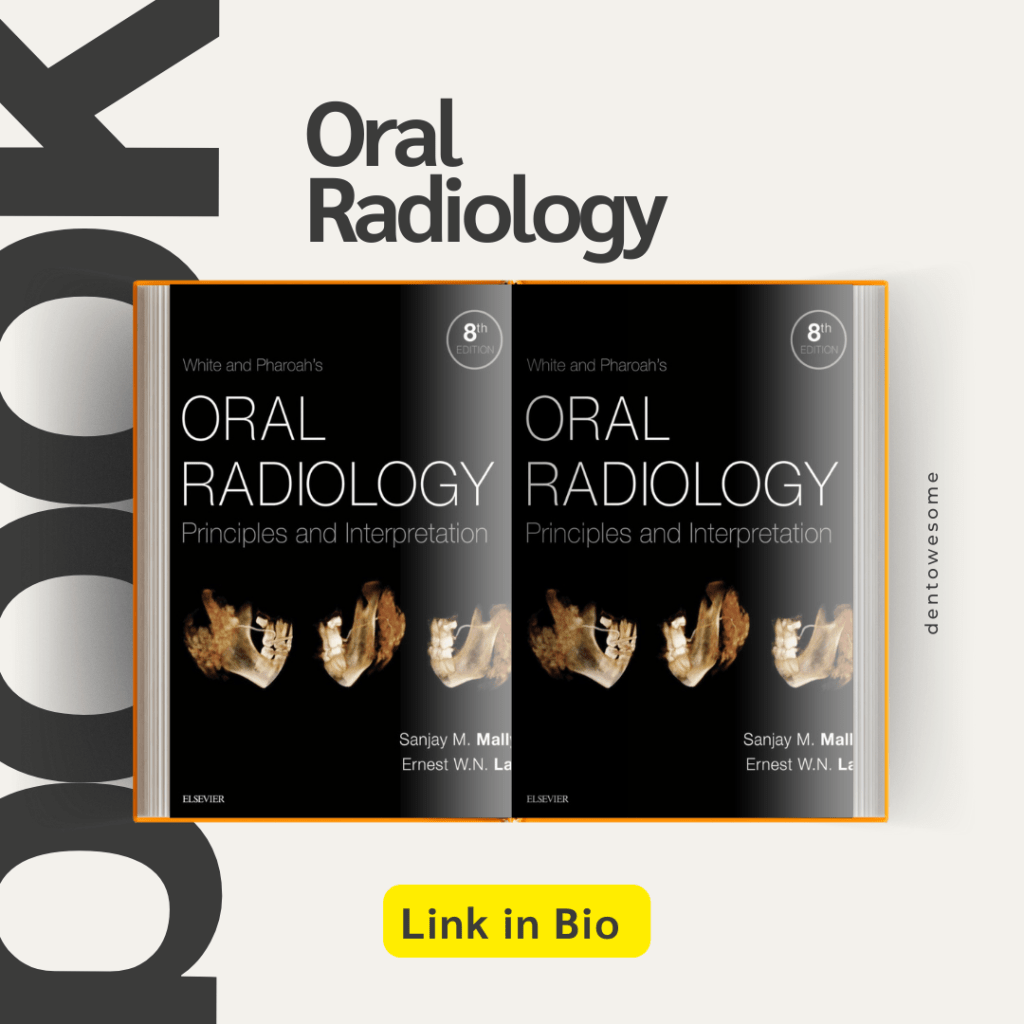
Intensive microbiologic, immunologic, and morphologic research investigations, especially during the past decade, have shown that colonization of tooth surface by pathogenic bacteria is accompanied by humoral and cellular defense mechanisms of the organism not only during the more advanced stage of infection, but also throughout the initial stages. Penetration of these complex defenses, which is usually of limited duration, disturbs the equilibrium of the system and results in disease. Within the dental pulp, this biologic equilibrium has to do with the balanced calcium and phosphate ion exchange during the continuous demineralization and remineralization of the enamel and exposed dentin. As long as a disease process is reversible, as is incipient caries, the capacity for progression and regression is present. Carious breakdown means that enamel is being demineralized by acidogenic plaque more rapidly than it can be remineralized. In its early stages, the caries has become a chronic destructive process, in which irreversible structural changes will preclude any further remission.
Looking at the dynamics of demineralization and remineralization, and the etiology of caries against the epidemiologic background, and comparing them with the results of therapy, a pattern of active disease spurts alternating with resting phases emerges. During these periods of remission, the chronic destructive process is not reversed, but is only brought to a standstill. This concept of progression and stagnation ( Socransky et al. 1984) is strongly influenced by the defensive capability of the organism.
Progression is defined by invasion of caries into dentin with inflammation and loss of connective tissue. Stagnation means the defenses are increased, there are defensive inflammatory cells in the tissues, and connective tissue is being replaced by secondary dentin or granulation tissue. Histologically, this ever-changing dynamic process in carious teeth is recorded over the years through deposition and destruction of dentin.
For the practitioner, the obvious questions that arise are how to classify the histopathologic condition of the pulp and the apical periodontal tissues, and how to initiate treatment that is appropriate, considering the background of stagnation or progression. Based upon clinical findings, differentiations are made between a clinically sound pulp, reversible pulpitis, irreversible pulpitis, a necrotic pulp, and apical periodontitis. These distinctions are based solely upon clinical observations; generally, a correlation between certain symptoms and a specific pathologic entity cannot be expected. Making the distinction between reversible and irreversible inflammations of the pulpal tissues can be a diagnostic problem, because they can present similar clinical symptoms. Histologically, the diagnosis of acute inflammation is based upon the predominance of neutrophilic granulocytes. However, this diagnostic picture does not always coincide with the appearance of pain symptoms because neutrophilic granulocytes can also be found in cases where there is no pain ( Langeland 1981, Lin and Langeland 1981 b, Lin et al. 1984 ).
Caries begins with microscopic demineralization of the affected enamel or cementum surface. As it progresses, the enamel first becomes chalky, then its surface is broken through. In this stage, the caries is easy to detect, but has frequently progressed so far that extensive restorative and endodontic treatment in necessary. More difficult to diagnose, on the other hand, are lesions that are in their early stages and dentinal lesions with macroscopically intact surfaces.
Epidemiologic studies have shown that – coincident with a general decrease in caries prevalence in industrialized countries – the occlusal surfaces of the permanent molars of children and young adults are the surfaces most frequently attacked by caries. In contrast to fissure caries, proximal and smooth surface caries is much less frequent. Radiographically evident incipient lesions in enamel of the proximal surfaces have likewise shown a decline. In adults, the probability that these lesions would penetrate further has increased, and this has caused the proportion of proximal caries to rise again.
During clinical examination using explorer many carious lesions with cavity go undiagnosed, so for their proper diagnosis bitewing radiographs, and fiberoptic transillumination (FOTI) are used. Bitewing radiographs are still the method of choice for the diagnosis of approximal caries, and account for the detection of approximately three-fourths of dentinal carious lesions ( Mileman and van der Weele 1990, Noar and Smith 1990). Studies found that where there is a dentinal lesion, there is a surface that has been broken through, which precludes any chance for remineralization (Marthaler and Germann 1970; Bille and Thylstrup 1982; Mejare and Malmgren 1986). Even though the actual extent of caries is underestimated with the radiograph, it may be concluded that the specificity, that is, the ability to recognize sound teeth as sound, is approximately 95% ( Mileman and van der Weele 1990). As far as caries diagnosis is concerned more sensitive X-ray films seem to be the equal of earlier films as far as caries diagnosis is concerned but as they produce same degree of contrast with significantly less radiation, their use is now highly recommended. Preventive measures can impede further penetration and even promote remineralization, provided that the enamel surface has not yet been disrupted.
The progression of caries can be monitored with periodic radiographs. Their interval depends, among other things, upon the individual’s susceptibility to caries. Patients at high risk of caries should be radiographed every year while those at very low risk need only be radiographed every 2-4 years. The time in which it takes caries to penetrate the enamel of a mature permanent molar in a patient with good oral hygiene can exceed 5 years. This offers the opportunity to post-pone invasive restorative treatment and to observe whether the caries progresses or regresses. The rate at which penetration progresses can be estimated by comparing radiographs produced at different times by a standardized technique. Recently erupted teeth, on the other hand, demonstrate a markedly reduced penetration time (Marthaler and Wiesner 1973, Shwarz et al. 1984).
In order to minimize overlapping of the images of approximating tooth surfaces, a film holder is recommended. A deviation of the horizontal angle of the X-ray tube by only a few degrees will result in a substantial decrease in correct diagnoses. Radiolucency in dentin should be treated as invasive only if there is also an unmistakable radiolucency in the enamel region. The radiograph should be inspected carefully under magnification and away from the influence of any light coming from the sides.
FOTI can be used in addition to bitewing radiographs if there is no interference from adjacent interproximal fillings that are other than tooth colored. More than 70% of dentinal lesions in anterior teeth can be detected by means of FOTI. Dentinal lesions in posterior teeth, however, can be differentiated only with great difficulty ( Pieper and Schurade 1987, Choski et al. 1994 ).

Reference – Color Atlas of Dental Medicine
ENDODONTOLGY
Rudolf Beer, Michael A. Baumann, and Syngcuk Kim
Nose is richly supplied by both the external and internal carotid systems, both on the septum and the lateral walls. NASAL SEPTUM Internal Carotid System – Branches of Ophthalmic Artery External Carotid System LATERAL WALL Internal Carotid System – Branches of Ophthalmic Artery External Carotid System LITTLE’S AREA Situated in the anterior inferior part of […]
A radiolucent lesion was found incidentally on a dental panoramic radiograph in a 30-year-old man. The cyst was located in the lower molar area above the inferior alveolar canal and showed a scalloped outline extending between the roots of the teeth. All teeth in the area were vital and the lamina dura was intact. Clear straw-coloured fluid was aspirated from the lesion


Solitary bone cyst (SBC), also known as simple bone cyst, is a benign bone lesion that most commonly occurs in children and adolescents. While the exact cause of SBC is still unknown, it is believed to be the result of a disturbance in the normal bone remodeling process.
SBC typically presents as a painless swelling or bump in the affected bone, often discovered incidentally on routine imaging. Diagnosis is usually made by imaging studies such as X-rays or MRI, as well as fine needle aspiration to confirm the presence of fluid within the cyst.
In many cases, SBCs will heal on their own without the need for any intervention. However, if the cyst is causing significant pain or functional impairment, or if it is at risk of fracturing or expanding and causing further damage to the bone, treatment may be necessary.
Treatment options for SBC include observation, which involves monitoring the cyst with regular imaging studies to ensure that it is not growing or causing any problems; curettage, which involves surgically removing the cyst and filling the cavity with bone graft material to promote healing; or injection of bone-stimulating agents such as bone morphogenetic protein (BMP) to promote healing and prevent recurrence.
The decision on whether to intervene or not will depend on various factors, including the size and location of the cyst, the age of the patient, and the presence of any associated symptoms or complications.
A 28-year-old woman presented for a check-up. The dentist noticed that the occlusal plane was depressed on the left side. The molar teeth did not make contact with the maxillary teeth on that side, though wear facets were present.

ANSWER
So, your jaw is made up of two parts called the maxilla (which is the upper part) and the mandible (which is the lower part). The mandible has a part called the ascending ramus on each side, which is a bony projection that helps to support the jaw joint.
Sometimes, one side of the ascending ramus can grow more than the other side. This is called condylar hyperplasia. It can cause the jaw to become uneven, with one side being bigger than the other.
When this happens, the teeth on the bigger side can grow more than the teeth on the smaller side. This can cause the teeth on the bigger side to stick out more and make the bite uneven.
Does that make sense to you? Let me know if you have any more questions!
1) Pouch and tunnel technique in conjunction with connective tissue Graft -a paramount for treating gingival recession
Gingival recession can be a bothersome and unappealing issue for patients. Thankfully, there’s an esthetic correction option available that’s both minimally invasive and promotes fast healing: the Pouch and Tunnel technique with connective tissue grafting (CTG). This approach is an excellent alternative for patients seeking effective recession coverage, and it’s worth considering if they are looking for a solution that’s both friendly to gums and their wallet.
Link – https://doi.org/10.21276/10.21276/ujds.2021.7.1.17
2) The natural tooth pontic and instant idea to retain aesthetics
In cases where a patient experiences sudden tooth loss in the anterior region of their mouth, it can be distressing and affect their confidence. The good news is that there are a range of treatment options available, including removable, tooth-supported, and implant-supported prosthetics.
Regardless of the chosen treatment, it’s important to restore the patient’s smile as quickly as possible while also stabilizing their dental arch. One technique involves using the patient’s own natural tooth as a pontic, which provides an exact match in terms of size, shape, and color, while also preserving the original 3D position of the tooth.
Link : https://www.hindawi.com/journals/crid/2016/8502927/
3) Modified roll technique- handy technique to augment the periimplant soft tissue in aesthetic zone
In this randomized controlled trial, researchers are exploring the effectiveness of a modified roll flap (MRF) technique to enhance the appearance of single-tooth implants in the esthetic zone. The MRF is a pedicle flap that utilizes the gingival tissue overlying the covering screw to thicken the labial soft tissue, which can have a significant impact on the overall esthetic outcome.
The study aims to measure the thickness of the labial soft tissue and the implant esthetic score system (IES) to evaluate the success of the MRF technique during stage-two implant surgery. By preserving and utilizing the existing tissue instead of discarding it, the MRF technique could potentially enhance the appearance of the implant site and improve patient satisfaction with the results.
Link: https://www.sciencedirect.com/science/article/pii/S1687857413000231
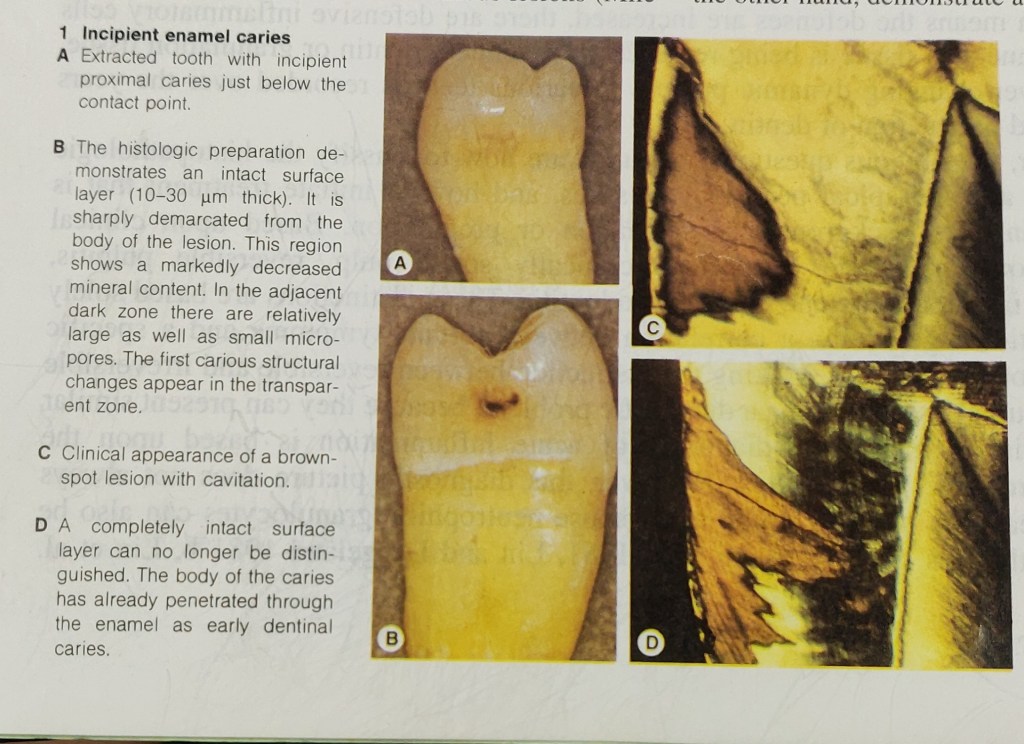
A 12-year-old female presented with a class II division 1 malocclusion on a moderate skeletal class II pattern, with increased vertical dimensions complicated by an increased overjet (12mm), crowding of both dental arches and teasing in relation to her dento-facial appearance.
What is treatment plan?

TREATMENT PLAN
1) Functional appliance like Dynamax or Twin block (more preffered as overjet reduction is more effective) = maxillary retroclination, mandibular incisor proclination, guides the eruption of posterior dentition.
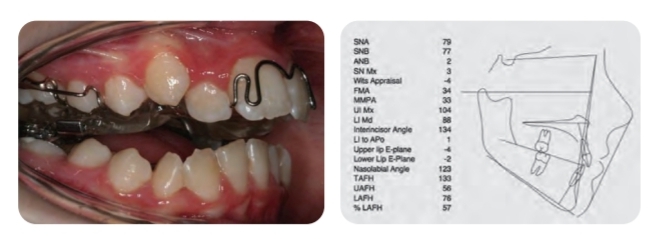
2) Need of Headgear with torqueing spurs = restricts maxillary forward growth and tipping of maxillary incisors.
3) Extraction of four second premolars followed by edge to edge appliances for stability of class II correction.

Highly elevated alkaline phosphatase is a good marker of Paget’s disease of bone in the appropriate clinical setting. Bone sequestration is often secondary to chronic osteomyelitis in the jaws. Bisphosphonates are used to treat Paget’s disease and also have been linked to jaw osteonecrosis.
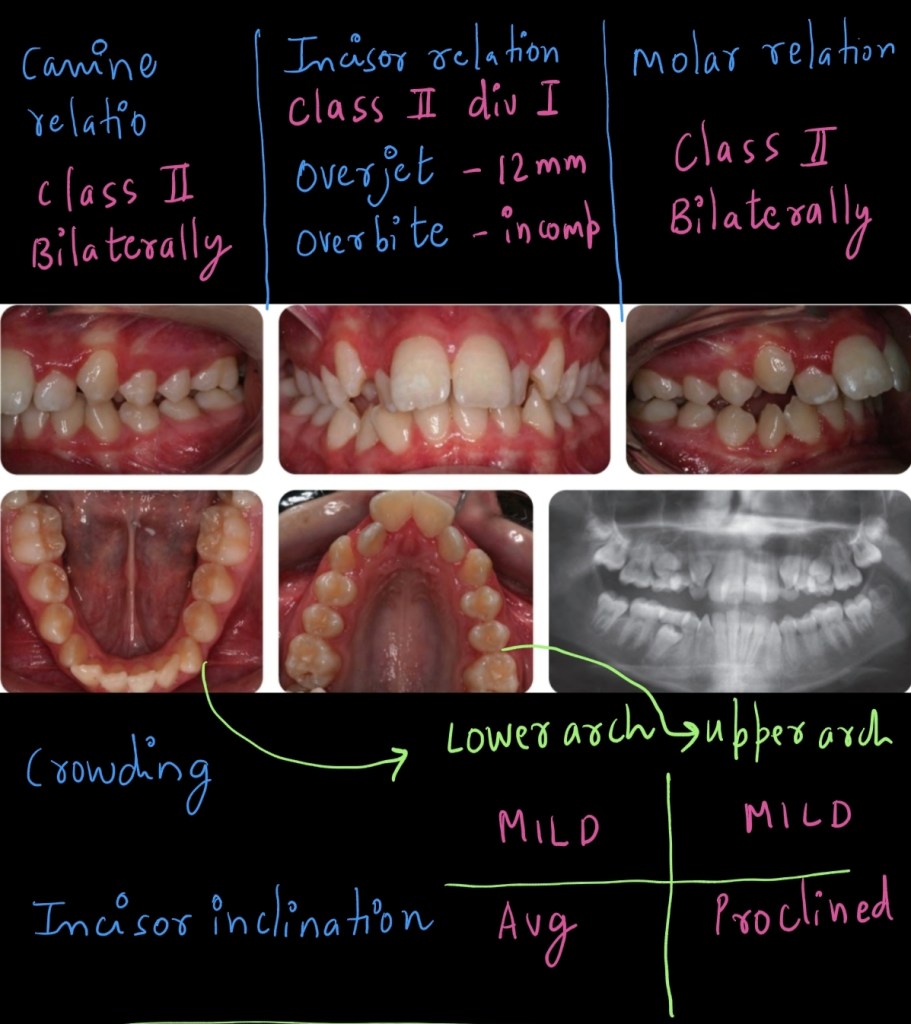
Study the two radiographs which are of the same
patient at (a) 19 years and (b) 34 years of age.
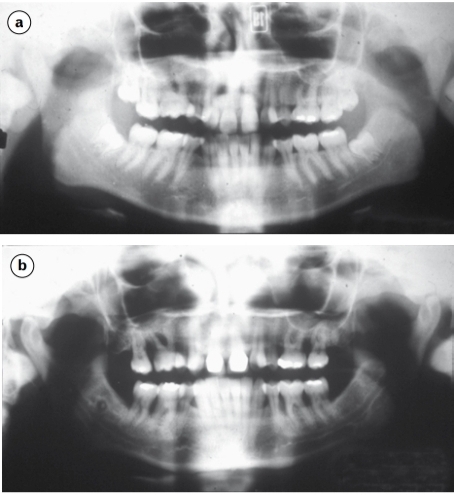
1 . What is the most likely periodontal diagnosis at 34
years of age?
Generalised aggressive periodontitis. The severity
of bone resorption and the radiographic absence of
signs of resorption at 19 years preclude a diagnosis of
chronic periodontitis.
2 . What does the initial phase of treatment involve?
Initially conventional cause-related treatment
is instigated: instruction in toothbrushing and
use of adjunctive aids for interproximal and
subgingival cleaning, RSI, prophylaxis. Ultimately,
treatments such as surgery and the adjunctive use of
antimicrobials might be indicated, but conventional
treatment is first in line.
3 . The patient has a sister who is aged 29 years. What
advice might you offer?
Periodontal screening and radiographic examination.
There is evidence that certain subjects are at high risk
from developing aggressive periodontitis and this
risk may be under genetic control. Siblings should
be screened and affected individuals with children
warned that early signs may develop from around
puberty onwards