Hey future orthodontists! 👋 Ready to dive deep into one of the most fascinating pieces of research in functional orthodontics? Today we’re breaking down Voudouris et al.’s groundbreaking study on condyle-fossa modifications during Herbst treatment. This isn’t just another research paper – it’s a paradigm shift that changes how we understand functional appliances!
Why This Research Matters 🎯
For decades, we’ve been taught that functional appliances work through lateral pterygoid muscle hyperactivity. But what if that’s completely wrong? This study flips the script and introduces the revolutionary Growth Relativity Theory.
Study Overview 📊
| Study Component | Details |
|---|---|
| Sample Size | 56 subjects total |
| Primate Subjects | 15 cynomolgus monkeys (Macaca fascicularis) |
| Human Subjects | 17 Herbst patients + 24 controls |
| Key Focus | 8 juvenile primates (24-36 months) |
| Treatment Duration | 6, 12, and 18 weeks |
| Activation Amount | 4-8mm progressive advancement |
The Revolutionary Methodology 🔬
What made this study special? Three cutting-edge techniques that previous research lacked:
1. Permanent EMG Electrodes 📡
- Old method: Temporary, transcutaneous electrodes
- New method: Surgically implanted permanent electrodes
- Muscles monitored: Superior and inferior lateral pterygoid, masseter, anterior digastric
2. Tetracycline Vital Staining 💡
- Intravenous tetracycline injection every 6 weeks
- Fluorescence microscopy with UV light
- Result: Crystal-clear visualization of new bone formation
3. Computerized Histomorphometry 🖥️
- Quantitative analysis of bone formation
- Measured area and thickness of new bone
- Statistical validation of results
The Shocking Results That Changed Everything 😱
What Everyone Expected vs. What Actually Happened
| Traditional Theory | Actual Findings |
|---|---|
| ⬆️ Lateral pterygoid hyperactivity | ⬇️ DECREASED muscle activity |
| Muscle-driven growth | Viscoelastic tissue-driven growth |
| Unpredictable results | Consistent, reproducible changes |
Key Findings Summary 📈
- Super Class I Malocclusion Development: All experimental subjects developed severe Class I relationships
- Glenoid Fossa Remodeling: Forward and downward growth (opposite to natural backward growth)
- Condylar Growth Enhancement: Increased mandibular length in all subjects
- Muscle Activity Paradox: Growth occurred with DECREASED EMG activity
The Growth Relativity Theory Explained 🧠
Think of it like this: Imagine the retrodiskal tissues as a giant elastic band 🎸 stretched between the condyle and fossa.
Displaced Condyle ←→ [Stretched Retrodiskal Tissues] ←→ Glenoid Fossa
↓ ↓
Radiating Growth Radiating Growth
Clinical Scenario 💭
Patient: 14-year-old with severe Class II, mandibular retrognathism
Traditional thinking: “The Herbst will make the lateral pterygoid muscles work harder to grow the condyle”
Reality: The Herbst creates reciprocal stretch forces that stimulate bone formation through mechanical transduction, not muscle hyperactivity!
Treatment Contributions Breakdown 📊
The researchers found that achieving a 7mm change along the occlusal plane involved multiple factors:
| Contributing Factor | Percentage Contribution |
|---|---|
| Condylar Growth | 22-46% |
| Glenoid Fossa Modification | 6-32% |
| Maxillary Changes | Variable |
| Dental Changes | ~30% |
| Total Orthopedic Effect | ~70% |
| Total Orthodontic Effect | ~30% |
Age-Related Treatment Response 🎂
Flowchart: Treatment Outcomes by Age
Patient Age Assessment
↓
┌─────────┴─────────┐
↓ ↓
Juvenile/Mixed Adolescent/Adult
Dentition Dentition
↓ ↓
High Condylar Limited Condylar
Growth Potential Growth Potential
↓ ↓
Significant Fossa Mainly Fossa
+ Condylar Changes Changes Only
Clinical Implications by Age 👶👦👨
| Age Group | Condylar Response | Fossa Response | Clinical Recommendation |
|---|---|---|---|
| Juvenile (Mixed Dentition) | High ✅ | High ✅ | Optimal treatment timing |
| Adolescent | Moderate ⚠️ | High ✅ | Good treatment timing |
| Adult | Limited ❌ | Moderate ⚠️ | Consider alternatives |
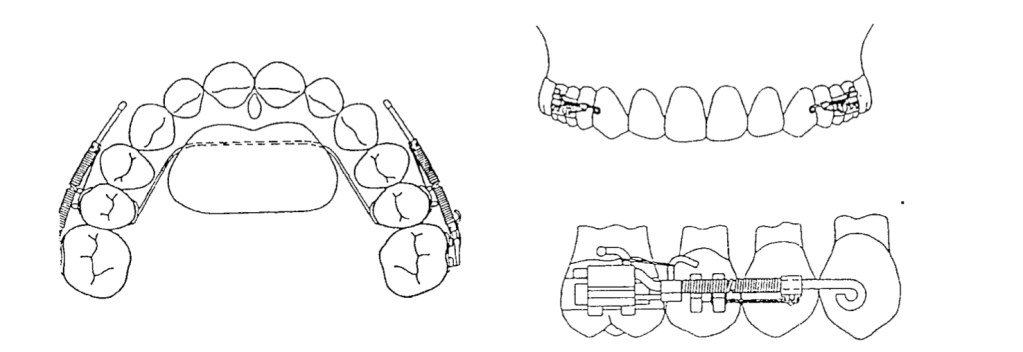
The Herbst-Block Design Innovation 🔧
Key design feature: 1.5mm posterior occlusal overlays
Why This Matters:
- Vertical distraction of condyle from articular eminence
- Prevents condylar resorption
- Avoids TMJ compression
- Optimizes stretch forces on retrodiskal tissues
Treatment Timeline and Bone Formation 📅
Progressive Changes Over Time
| Time Point | Bone Formation Area | Key Observations |
|---|---|---|
| 6 weeks | Early changes | Extensive cartilage proliferation |
| 12 weeks | 1.2mm average | Peak bone formation rate |
| 18 weeks | Maximum response | Doubled postglenoid spine thickness |
Correlation: r = 0.95 between treatment time and bone formation! 📈
Clinical Decision-Making Flowchart 🗺️
Class II Patient Evaluation
↓
Age Assessment
↓
┌─────────┴─────────┐
↓ ↓
Mixed Dentition Permanent Dentition
↓ ↓
Herbst with Consider Herbst vs
Occlusal Coverage Alternative Treatment
↓ ↓
Continuous Monitor for:
Activation - Condylar resorption
1-2mm every - Disk displacement
10-15 days - Relapse potential
Key Clinical Takeaways for Practice 💡
Do’s and Don’ts
| ✅ DO | ❌ DON’T |
|---|---|
| Use continuous activation | Rely on intermittent wear |
| Include occlusal coverage | Ignore vertical dimension |
| Monitor for 6+ months | Expect immediate results |
| Plan retention carefully | Assume permanent changes |
Red Flags to Watch For 🚩
- Condylar resorption – prevented by proper vertical dimension
- TMJ pain – indicates excessive compression
- Rapid relapse – inadequate retention period
- Disk displacement – poor appliance design
The Retention Challenge 🔄
Critical Finding: Without adequate retention, positive condyle-fossa changes can relapse due to:
- Return of anterior digastric muscle function
- Perimandibular connective tissue pull
- Natural tendency for condyle to seat posteriorly
Retention Protocol Recommendations:
- Minimum 6 months active retention
- Progressive reduction of appliance wear
- Monitor muscle reattachment process
- Long-term follow-up essential
Clinical Scenario Application 🎯
Case: 13-year-old female, Class II Division 1, severe mandibular retrognathism
Treatment Plan Based on Research:
- Herbst with occlusal coverage (NOT standard Herbst)
- Progressive activation 1.5mm every 2 weeks
- 12-week minimum treatment duration
- Expect 70% orthopedic response
- Plan extended retention phase
Expected Outcomes:
- Forward fossa remodeling
- Increased mandibular length
- Super Class I result requiring finishing
- Need for comprehensive retention protocol
Future Implications 🔮
This research suggests that functional appliances should be renamed “dentofacial orthopedic appliances” because they work through:
- Viscoelastic tissue forces
- Mechanical transduction
- Growth modification, NOT muscle function
Study Limitations and Considerations ⚖️
Strengths:
- Rigorous methodology with multiple validation techniques
- Control groups and statistical analysis
- Novel technological approaches
Limitations:
- Animal model – translation to humans requires validation
- Small sample size – justified but limits generalizability
- Short-term follow-up – long-term stability unknown
Conclusion: Changing Clinical Practice 🎯
This groundbreaking research fundamentally changes how we understand functional appliances. The key shifts in thinking:
- From muscle hyperactivity → To tissue stretch forces
- From unpredictable results → To consistent orthopedic changes
- From simple tooth movement → To complex TMJ remodeling
- From empirical treatment → To evidence-based protocols
Memory Aid for Boards 📚
“VOUDOURIS RULES” 🧠
- Viscoelastic forces drive change
- Occlusal coverage prevents resorption
- Undermining old muscle theories
- Decreased EMG activity during growth
- Orthopedic effects dominate (70%)
- Underaged patients respond best
- Retention critical for stability
- Inferior-anterior fossa growth
- Super Class I results expected
Questions for Self-Assessment 🤔
- What percentage of Herbst treatment effects are orthopedic vs orthodontic?
- Why does EMG activity decrease during successful treatment?
- What prevents condylar resorption in Herbst appliances?
- At what age is condylar growth potential highest?
- What is the Growth Relativity Theory?
Remember: This research doesn’t just change what we know about Herbst appliances – it revolutionizes our understanding of functional orthodontics entirely! 🚀
Keep studying, future orthodontists! The field is constantly evolving, and staying current with research like this will make you better clinicians. 📖✨