
Dr. Mehnaz Memon🖊
References: Davidson’s Principles and Practice of Medicine Textbook



Dr. Mehnaz Memon🖊
References: Davidson’s Principles and Practice of Medicine Textbook

Source- textbook of pathology for dental students Ramdas Nayak and pinterest

Source – textbook of pathology for dental students Ramdas Nayak and Google images


Source- textbook of pathology for dental students Ramdas Nayak and Google images
Source- textbook of pathology for dental students Ramdas Nayak and Google images
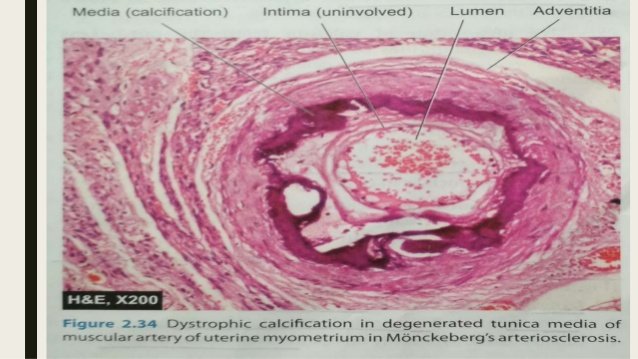

Source – textbook of pathology for dental students Ramdas Nayak and Google images
Acute hepatitis
Chronic hepatitis

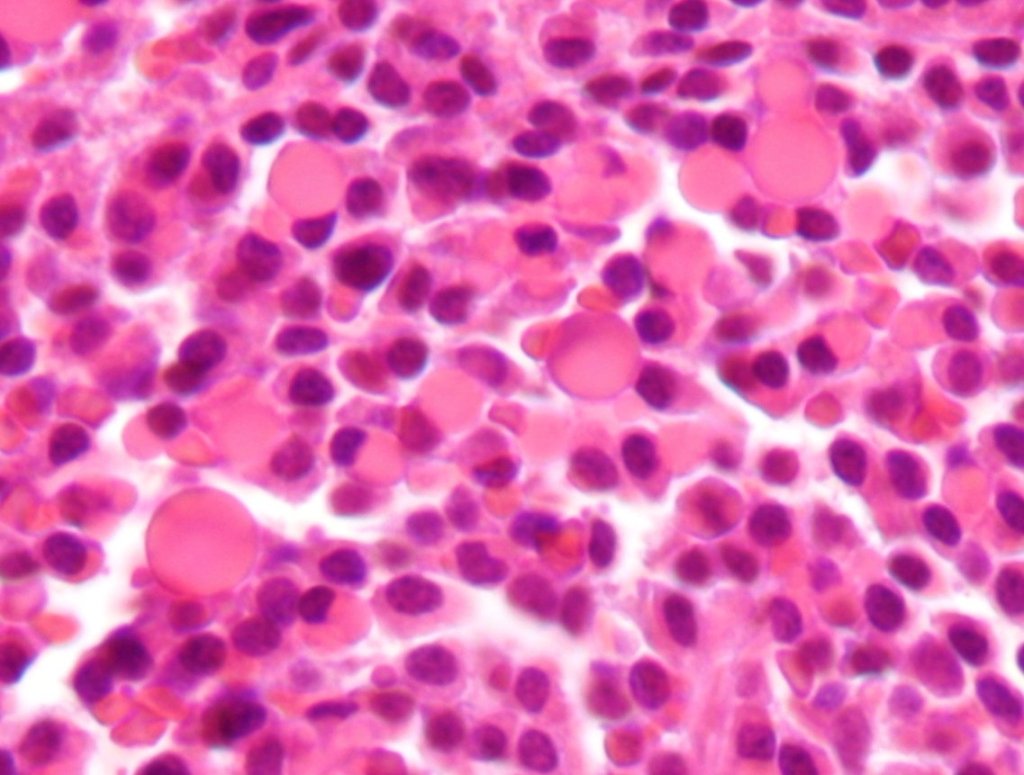
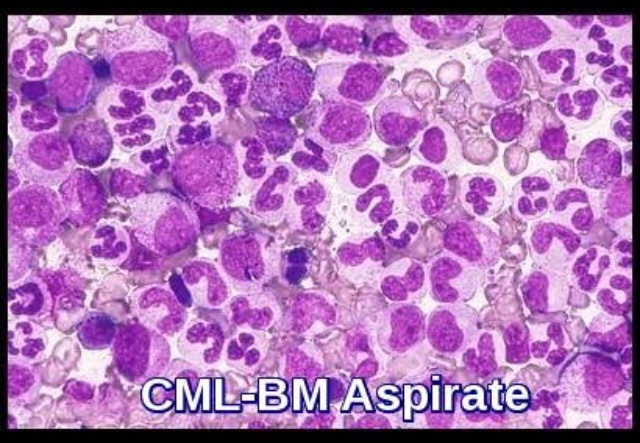
Leukemias are malignant Neoplasms of the haematopoetic stem cells characterized by diffused replacement of bone marrow by Neoplastic cells with or without involvement of the peripheral blood.
➡️ Chronic leukaemia is a disease of insidious onset, affecting middle aged & young adults (CML)
🔘 1 lakh - 5 lakh/cu.mm
🔘 Differential count reveals more mature forms in Peripheral smear, complete spectrum of granulocytes, myelocytes & band cells (50%)
🔘 Blast cell > 10% of leukocytes
🔘 Phases:
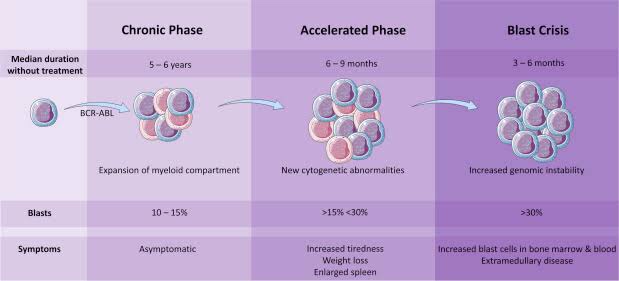
1. Chronic phase:
➡️ Myeloproliferative disorder – excessive proliferation of myeloid cells & mature segmented Neutrophils
➡️ Basophils upto 10% (feature of CML)
2. Accelerated phase:
3. Blastic phase: Myeloid blast crisis in CML resembles AML >20%
• neutrophil alkaline phosphatase (NAP) activity is markedly reduced in CML
🔘 Splenectomy and splenic irradiation have been used in patients with large and painful spleens, usually in the late phase of CML. This is rarely needed in patients whose disease is well controlled.
🔘 For those patients unable to tolerate chemotherapy, leukapheresis is a viable option.
Dr. Mehnaz Memon🖊
References: