
Source- textbook of oral pathology Shafers and Google images

Source- textbook of oral pathology Shafers and Google images



Source- textbook of oral pathology Shafers and Google images



Source- textbook of oral pathology Shafers and Google images
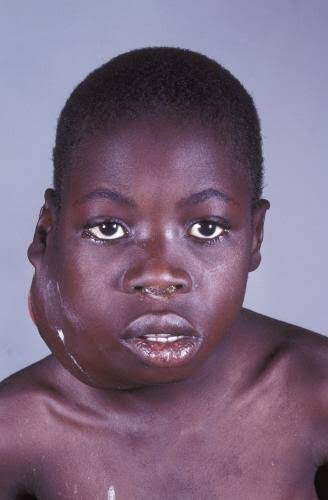
It is also called as ‘African jaw lymphoma’. It is a lymphoreticular cell malignancy. In the African form jaw involvement is 75% and in cases of the American form, abdomen involvement is more common. It is a B-cell neoplasm.
Etiology
• Epstein-Barrvirus(EBV)which also causes nasopharyn- geal carcinoma and infectious mononucleosis is considered to be the etiological factor. There are higher EBV antibody levels in patients of Burkitt’s lymphoma.
Clinical Features
Oral Manifestations
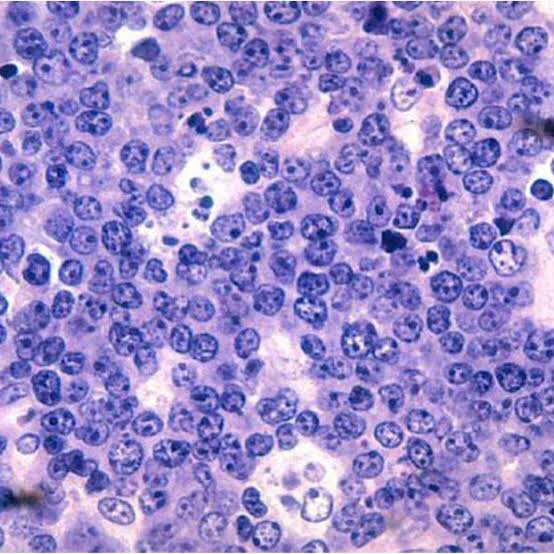
Histology
Shows characteristic starry sky appearance.

• Radiological diagnosis—moth eaten appearance is seen with loss of lamina dura around the teeth.
• Laboratorydiagnosis—monotonous sea of un differentiated monomorphic lymphoreticular cells, usually showing abundant mitotic activity. There is also hyperchro- matosis and loss of cohesiveness. Characteristic ‘starry sky’ appearance is seen.
Management
• Cytotoxicdrugs—cytotoxicdrugs like cyclophosphamide 40 mg/kg in single IV administration and repeated about 2 weeks later. Vincristine and methotrexate have been successful in some cases.
• Multiagent chemotherapy—combination of drugs such as cyclophosphamide, vincristine and methotrexate give better results than any single drug. Majority of patients show dramatic response to the therapy. The swelling regresses and the displaced teeth return to their normal position within 1 to 2 weeks.
REFERENCE- SHAFER’S TEXTBOOK OF ORAL PATHOLOGY AND ANIL GHOM TEXTBOOK OF ORAL MEDICINE
Intrinsic Stains
Pre-eruptive Causes
These are incorporated into the deeper layers of enamel and dentin during odontogenesis and alter the development and appearance of the enamel and dentin
.Alkaptonuria: Dark brown pigmentation of primary teeth is commonly seen in alkaptonuria. It is an autosomal recessive disorder resulting into complete oxidation of tyrosine and phenylalanine causing increased level of homogentisic acid.
Hematological disorders
• Erythroblastosis fetalis: It is a blood disorder of neonates due to Rh incompatibility. In this, stain does not involve teeth or portions of teeth developing after cessation of hemolysis shortly after birth. Stain is usually green, brown or bluish in color.

• Congenital porphyria: It is an inborn error of por- phyrin metabolism, characterized by overproduction of uroporphyrin. Deciduous and permanent teeth may show a red or brownish discoloration. Under ultraviolet light, teeth show red fluorescence.

• Sickle cell anemia: It is inherited blood dyscrasia characterized by increased hemolysis of red blood cells. In sickle cell anemia infrequently the stains of the teeth are similar to those of erythroblastosis fetalis, but discoloration is more severe, involves both dentitions and does not resolve with time.
Amelogenesis imperfecta: It comprises of a group of conditions, that demonstrate developmental alteration in the structure of the enamel in the absence of a systemic disorders. Amelogenesis imperfecta (AI) has been classified mainly into hypoplastic, hypocalcified and hypomaturation type.

Fluorosis: In fluorosis, staining is due to excessive fluoride uptake during development of enamel. Excess fluoride induces a metabolic change in ameloblast and the resultant enamel has a defective matrix and an irregular, hypomineralized structure



Posteruptive Causes

– Dentin deposition: Secondary and tertiary dentin deposits, pulp stones cause changes in the color of teeth.
• Functional and parafunctional changes: Tooth wear may give a darker appearance to the teeth because of loss of tooth surface and exposure of dentin which is yellower and is susceptible to color changes by absorption of oral fluids and deposition of reparative dentin.
Extrinsic Stains
Daily Acquired Stains
Plaque: Pellicle and plaque on tooth surface gives rise to yellowish appearance of teeth.
Food and beverages: Tea, coffee, red wine, curry and colas if taken in excess cause discoloration.
Tobacco use results in brown to black appearance of teeth.
Poor oral hygiene manifests as:
Swimmer’s calculus:
– It is yellow to dark brown stain present on facial andlingual surfaces of anterior teeth. It occurs due toprolonged exposure to pool water.
Gingival hemorrhage.
Chemicals
• Chlorhexidine stain: The stains produced by use of chlorhexidine are yellowish brown to brownish in nature.
Metallic stains: These are caused by metals and metallic salts introduced into oral cavity in metal containing dust inhaled by industry workers or through orally administered drugs.

Stains caused by different metals
• Copper dust—green stain
• Iron dust—brown stain
• Mercury—greenish black stain • Nickel—green stain
• Silver—black stain.
Reference- Nisha garg textbook of endosontics and Anil Ghom textbook of oral medicine

A supernumerary tooth is an additional tooth to the normal set of teeth. It may closely resemble the teeth of the group to which it belongs, i.e, molars, premolars or anterior teeth, or it may bear little resemblance in size or shape to the teeth with which it is associated.
It is also called as ‘hyperdontia’. It is defined as any tooth or tooth substance in the excess of the usual configuration of twenty deciduous or thirty two permanent teeth.
Pathogenesis and etiology
Four different morphological types of supernumerary teeth have been described:
• Conical
• Tuberculate
• Supplemental
• Odontome
Conical. This small peg-shaped conical supernumerary tooth is most commonly found in the permanent dentition. It develops with root formation ahead of or at an equivalent stage to that of permanent incisors and usually presents as a mesiodens. The conical supernumerary can result in rotation or displacement of the permanent incisor, but rarely delays eruption.

Tuberculate. The tuberculate type of supernumerary possesses have more than one cusp or tubercle. It is frequently described as barrel-shaped and may be invaginated. Root formation is delayed compared to that of the permanent incisors. Tuberculate supernu- meraries are often paired and are commonly located on the palatal aspect of the central incisors. They rarely erupt and are frequently associated with delayed eruption of the incisors.

Supplemental. The supplemental supernumerary refers to a duplication of teeth in the normal series and is found at the end of a tooth series. The most common supplemental tooth is the permanent maxillary lateral incisor, but supplemental premolars and molars also occur. The majority of supernumeraries found in the primary dentition are of the supplemental type and seldom remain impacted.
Odontome. The term ‘odontoma’ refers to any tumour of odontogenic origin. Odontoma represents a hamartomatous malformation rather than a neoplasm. The lesion is composed of more than one type of tissue and consequently has been called a composite odontoma. Two separate types have been described, the diffuse mass of dental tissue which is totally disorganized is known as a complex composite odontoma; whereas, the malformation which bears some superficial anatomical similarity to a normal tooth is referred to as a compound composite odontoma.

According to location
• Mesiodens—it is located at or near the midline in the incisal region of maxilla between central incisors . It is a small tooth with cone shaped crown and short root. It may cause retarded eruption, displacement or resorption of adjacent root. It frequently causes improper alignment.

• Distomolar—it is found in molar region frequently located distal to 3rd molar. Generally, these teeth are smaller than normal 2nd and 3rd molar, crown morphology is highly abnormal.
• Paramolar—it is supernumerary molar, usually small and rudimentary and is situated buccally or lingually to one of the maxillary molars or interproximally between 1st, 2nd and 3rd maxillary molars.

• Peridens—supernumerary teeth that erupt ectopically, either buccally or lingually to the normal arch are referred as peridens.
Radiographic features

When it is needed—if abnormal clinical signs are present you can go for OPG examination, IOPA, occlusal radiographic examination.
Significance—radiograph will aid in determining the location and number of unerupted teeth. It can also used to see if there is any cyst formation.
Appearance—theirradiographicpictureischaracteristic of teeth.
Management
• Surgical extraction—it depends on potential effect on normal dentition, their position, number and complications that may result from surgical removal. If required, they should be extracted.
REFERENCE- SHAFER’S TEXTBOOK OF ORAL PATHOLOGY 8TH ED AND ANIL GHOM TEXTBOOK OF ORAL MEDICINE TEXTBOOK OF ORAL MEDICINE
Also called as scrotal tongue and lingua plicata
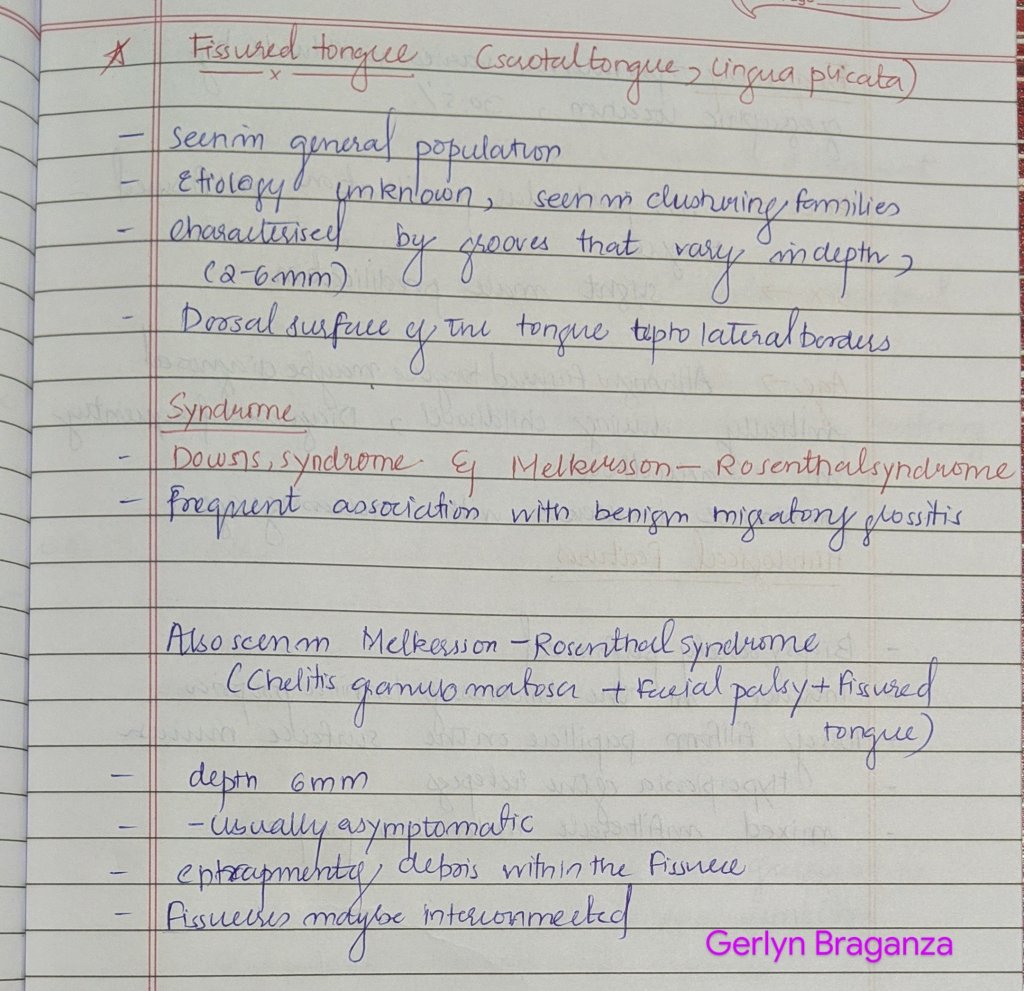


Source- textbook of oral pathology Shafers and Google images
Also called as bifid tongue



Source – textbook of oral pathology Shafers and Google images
Also called as Tongue Tie


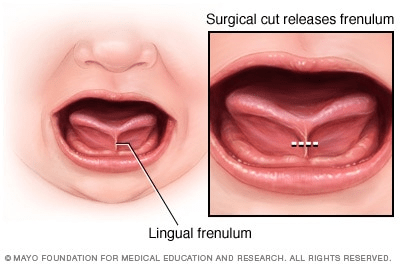
Source- textbook of oral pathology Shafers and Google images
Also called as Tongue Hypertrophy, Prolapsus of the tongue, Enlarged Tongue and Pseudomacroglossia


Source- textbook of oral pathology Shafers and Google images