Molar distalization is a crucial technique in orthodontics, particularly for patients with Class II malocclusion. Thanks to advancements in biomechanics, materials, and technology, orthodontists now have access to a variety of intramaxillary intraoral appliances that can apply light, continuous forces for effective molar distalization. These appliances have become a game-changer, providing us with more precise control and predictable results.
Types of Intramaxillary Appliances
The application of forces in molar distalization can come from two primary areas: the buccal or the palatal region. Depending on where the force is applied, appliances can be categorized into two broad groups:
- Buccal Force Application: These appliances apply force from the outside of the dental arch.
- Palatal Force Application: These appliances exert force from the roof of the mouth.
Additionally, the force mechanisms can be divided into two categories:
- Friction-Free Mechanism: This type involves appliances like the pendulum, which are designed to move the molars without causing significant friction.
- Sliding Mechanism: Appliances like nickel-titanium (NiTi) coil springs use a sliding mechanism to apply force, creating a more dynamic force delivery system.
Each of these appliance types has its own set of advantages and drawbacks, and comparing their efficiency in achieving molar distalization is key to making evidence-based treatment decisions. However, due to the limited number of randomized clinical trials, a meta-analysis is often not possible. That said, a comprehensive analysis of existing studies can still offer valuable insights into how these appliances work.
Treatment Outcomes: Overall Effects
When all intramaxillary appliances were considered together, some general findings emerged:
- First Molar Movement: On average, first molars moved 2.9 mm distally, but this came with a 5.4° of distal tipping.
- Incisor Movement: The incisors shifted mesially by 1.8 mm with 3.6° of mesial tipping.
- Premolar Movement: Premolars showed a mesial shift of 1.7 mm, though tipping was less pronounced.

Vertical movements were generally extrusive for incisors and premolars, with incisors showing an average extrusion of 0.4 mm and premolars 1.1 mm. Interestingly, molar vertical movements were not statistically significant, indicating that the main effect on molars was distal movement and tipping rather than vertical displacement.
Treatment Effects: Buccal vs. Palatal Appliances
Now, let’s delve into the specific effects of buccal and palatal appliances. These results highlight the different ways these appliances move teeth:
- Buccal Appliances:
- Molar Movement: Molar distal movement was 2.6 mm, with a more significant tipping of 8.3°.
- Incisor Movement: Incisors moved mesially by 1.9 mm with 5.0° of mesial tipping.
- Premolar Movement: Premolars demonstrated a 2.0 mm mesial shift, accompanied by 7.0° of mesial tipping.
- Vertical Movement: Premolars showed a slight extrusion of 0.7 mm, while incisors had a more modest extrusion of 0.2 mm.

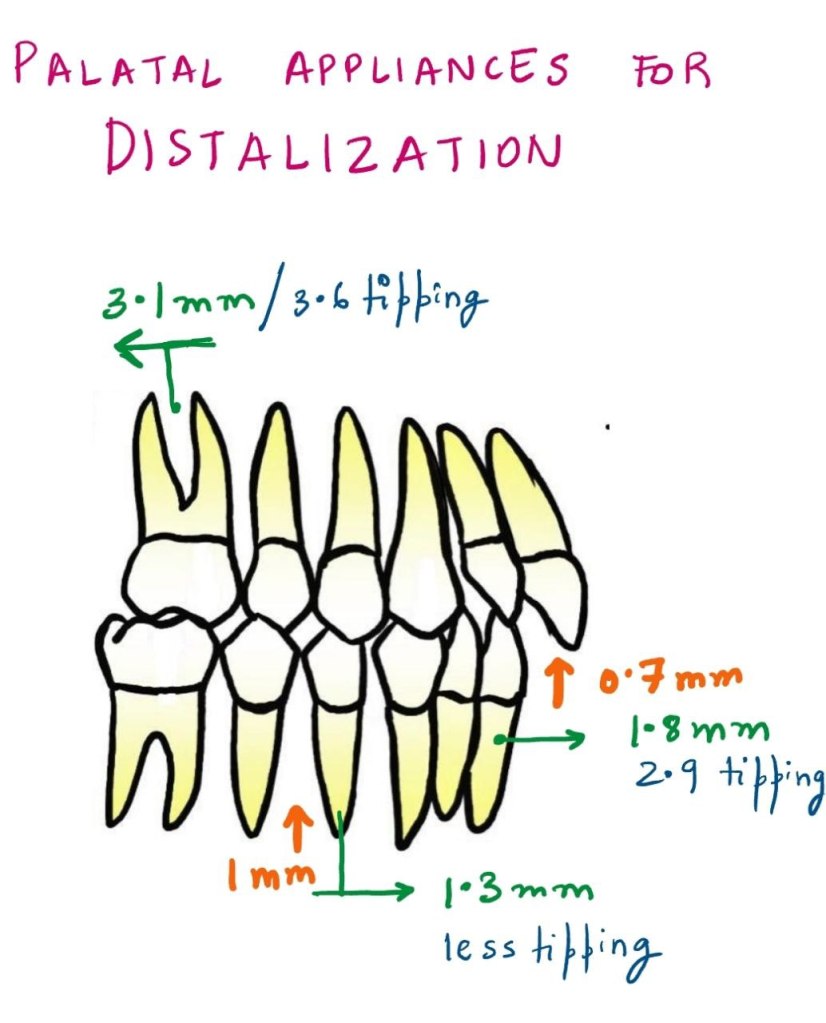
- Palatal Appliances:
- Molar Movement: Molar distalization was slightly more pronounced, with 3.1 mm of movement and 3.6° of tipping.
- Incisor Movement: Incisors exhibited a mesial shift of 1.8 mm with 2.9° of mesial tipping.
- Premolar Movement: Premolars moved mesially by 1.3 mm with less tipping than buccal appliances.
- Vertical Movement: The extrusion for incisors was 0.7 mm, and premolars showed an extrusion of 1.0 mm.
Molar Distalization and Anchorage Loss
The primary effect of noncompliance intramaxillary appliances is molar distalization, which is typically achieved through a combination of crown distal movement and tipping. While distalization is the goal, a common side effect observed is loss of anchorage. This loss can be seen in the mesial movements and extrusions of incisors and premolars.
Key Findings:
- Molars: Show a combination of distal crown movement and distal tipping.
- Incisors: Exhibit mesial movement, tipping, and extrusion.
- Premolars: Display mesial crown movement and extrusion.
As with any treatment modality, careful planning is required to manage these unintended side effects and achieve the best possible clinical outcomes.
Buccal vs. Palatal Appliances: Tipping and Force Mechanics
One interesting observation in the study was the difference in tipping effects between buccal and palatal acting appliances. Palatal appliances consistently resulted in less tipping of teeth compared to buccal appliances, as indicated by the non-overlapping confidence intervals.
Why the Difference?
The key reason for this difference lies in the moment arm of the force. In palatal appliances, the line of action of the force is closer to the center of resistance of the tooth, leading to less tipping and more controlled molar movement.
Table 1: Comparison of Tipping between Buccal and Palatal Appliances
| Appliance Type | Molars Distal Movement (mm) | Molars Tipping (°) | Incisor Mesial Movement (mm) | Incisor Tipping (°) | Premolar Mesial Movement (mm) | Premolar Tipping (°) |
|---|---|---|---|---|---|---|
| Buccal Appliances | 2.6 | 8.3 | 1.9 | 5.0 | 2.0 | 7.0 |
| Palatal Appliances | 3.1 | 3.6 | 1.8 | 2.9 | 1.3 | 3.0 |
This table highlights the greater tipping observed with buccal appliances compared to palatal appliances, as well as the differences in molar distalization and mesial movement of incisors and premolars.
The Nance Button: Anchorage Considerations
Another point of discussion is the use of the Nance button to reinforce anterior anchorage during molar distalization. While it can support anchorage to some extent, it does not provide absolute anchorage. This is because the Nance button, as part of the anchorage unit, cannot completely resist mesial forces during molar distalization. Clinically, this often results in an increased overjet and proclination of maxillary incisors.
Clinical Tip:
For patients already presenting with an increased overjet, orthodontists must proceed with caution when prescribing these appliances. These cases may require additional measures to control the overjet and manage incisor proclination.
The Pendulum Appliance: A Look at Tipping and Movement
The pendulum appliance, a popular friction-free appliance, was noted in the study to cause the greatest distal tipping of molars. However, this tipping was correlated with a larger amount of distal crown movement. Interestingly, this tipping can often be corrected with the use of molar uprighting bends.
Table 2: Molar Distalization and Tipping with the Pendulum Appliance
| Movement Type | Molar Distal Movement (mm) | Molar Tipping (°) |
|---|---|---|
| Pendulum Appliance | 3.4 | 9.0 |
This table shows that the pendulum appliance can achieve significant molar distalization but at the cost of increased tipping. These tipping movements can be addressed with molar uprighting bends, which can help reduce the tipping angle.
Factors Affecting Molar Distalization
Several factors can influence the effectiveness of molar distalization, including:
- Teeth Used for Anchorage: Different anchorage setups can affect the extent of distal movement.
- The Type of Appliance Used: Whether the appliance uses a sliding mechanism or a friction-free mechanism plays a role.
- Patient Factors: Age, initial molar relationships, and the eruption of second and third molars all contribute to how effectively molars are distalized.
In studies that focus on growing patients, mean ages ranged from 11.2 to 14.9 years, which is crucial because the growth phase can significantly impact the effectiveness of treatment. For example, molar distalization is often more effective before the second molars have erupted. When second molars are erupted, more force may be required, and the treatment time may increase.
Table 3: Influence of Molar Eruption on Distalization Efficiency
| Condition | Molar Distalization Efficiency |
|---|---|
| Second Molars Unerupted | More efficient, faster results |
| Second Molars Erupted | Less efficient, longer treatment |