Every smile has a story, and so does every dentist who crafts them. In this exclusive conversation, we sit down with Dr. Anchal Shah, Prosthodontist at Dr. Shah’s Smile Studio, to learn about her inspiring journey—from a childhood fascination with chocolates to rebuilding lives through maxillofacial prosthetics.
1) Can you share how your path in the dental profession began and the key milestones that shaped it?
✨ Childhood:
It’s funny how a simple love for chocolates led me toward a world I never imagined—dentistry. What began as curiosity slowly transformed into passion.
✨ BDS Days:
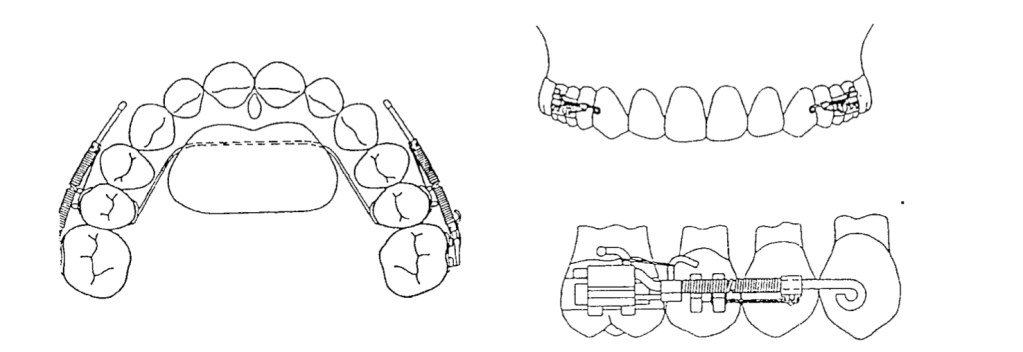
The first two years were honestly tough. I often felt lost, wondering why I was spending hours working on baseplates or burning my fingers. But once clinics began, everything changed. I discovered joy in the smallest things—making dentures, performing extractions, or the adrenaline rush of placing my first suture.
✨ The Big Leap:
I always dreamt of specializing in Prosthodontics. My first NEET MDS attempt didn’t work out, but I refused to give up. Taking a drop year was challenging, but it became one of the best decisions of my life. The effort paid off with AIR 66and admission to my dream college.
✨ Shaping My Purpose:
Training under legends in Maxillofacial Prosthodontics gave me a mission bigger than myself—helping oral cancer survivors regain not just their smile, but their confidence and dignity.
✨ Where I Am Today:
At Dr. Shah’s Smile Studio, I blend skill with compassion. My approach is holistic—every smile matters, every pain deserves care, and every patient’s story reminds me why I chose this path.

2) What inspires you to stay passionate and committed to dentistry, even during challenging times?
Dentistry, like life, isn’t always smooth. Some days are tough—when cases get complicated, outcomes don’t go as planned, or the weight of responsibility feels overwhelming.
On those days, I remind myself of two things:
🌱 How far I’ve come:
From a confused BDS student burning my fingers on a baseplate to securing AIR 66 and finding my calling in Prosthodontics—every struggle has shaped me.
💡 Why I started:
It was never just about teeth. It’s always been about people—their pain, their confidence, and their smiles. Watching a patient smile again after years is the kind of reward that keeps me going.
Every difficult moment becomes lighter when I remind myself of this:
👉 I didn’t come this far to give up. I came this far to make a difference

3) Who is your role model in the dental field and how has this person influenced your approach to patient care, academics, or professional growth?
I owe so much to my mentors.
• Dr. Rupal Shah, my postgraduate guide and Head of Department, taught me how much can be achieved with so little in hand. Her resourcefulness and patient-centered care continue to inspire my daily practice.
• Dr. P. C. Jacob, my mentor in oral cancer rehabilitation, showed me the power of perseverance and empathy in dealing with some of the most complex and emotionally demanding cases.
Their teachings shaped my outlook—not just as a clinician, but as a human being who believes in healing beyond treatment.

4) Could you discuss the strategies you use to manage academic responsibilities alongside your personal interests or hobbies?
Dentistry can easily consume your entire day, but I’ve learned that balance is key. Keeping my small passions alive keeps me grounded.
For me, it’s listening to podcasts, tuning into music, or watching a good movie.
Podcasts give me new perspectives, music uplifts my mood instantly, and movies help me pause and reset.
Even 20–30 minutes a day can make a difference. You don’t need hours for hobbies—just intention.
These little joys refill my energy, empathy, and creativity, helping me return to dentistry with a refreshed mind.
Because while dentistry defines my work, my hobbies remind me who I am.

5) What advice would you give to current dental students and aspiring dentists?
Don’t rush to have it all figured out. It’s completely normal to feel lost in the beginning—to question your path, or to wonder why you’re spending endless hours perfecting a baseplate or bending wires.
Trust the process. Those small, repetitive tasks are building your foundation—your patience, precision, and perseverance.
Stay consistent. Stay curious. And don’t fear setbacks. One exam, one failure, or one tough day doesn’t define your journey—your persistence does.
Most importantly, never forget why you started.
Dentistry is not just about teeth—it’s about people, their confidence, and their smiles.