A chronic, autoimmune, sub-epidermal blistering skin disease that rarely involves mucous membrane.

🔹Clinical Features:
Age: Elderly (>60 years)
Skin Lesions:
- Generalised non-specific rash, commonly on Limbs.
- Appears urticarial/eczematous; persist for several weeks to months.
- Vesicles & bullae arise in prodromal skin lesion as well as Normal skin.
- The blisters are thick walled and don’t rupture easily.
- ruptured blisters are usually sensitive and painful, have raw eroded area which heals rapidly.
Oral Manifestations:
Vesicles appear gingivally👇🏻

Erythematous & desquamate as result of minor frictional trauma
👉🏻 Oral lesions comprise of bullae/vesicle that rupture to form erosions and ultimately leave out ulcerations
👉🏻 Other sites:
- Buccal Mucosa
- Tongue
- Floor of the mouth
- Palate

🔹Diagnosis:
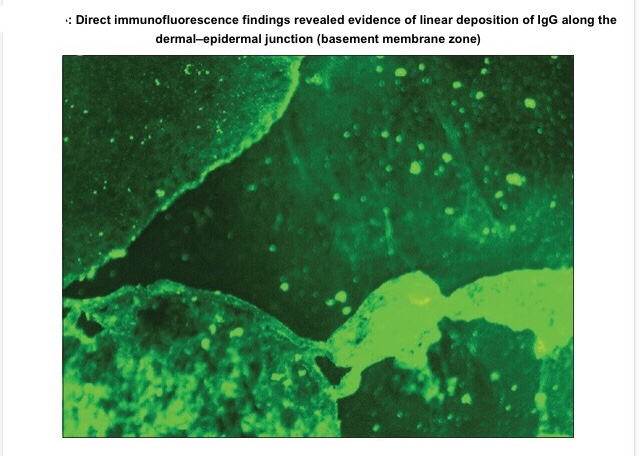
Apart from evaluating history, clinical presentation, histopathological analysis is carried out followed by direct immunofluorescence study for the differential diagnosis and confirmation of the condition.
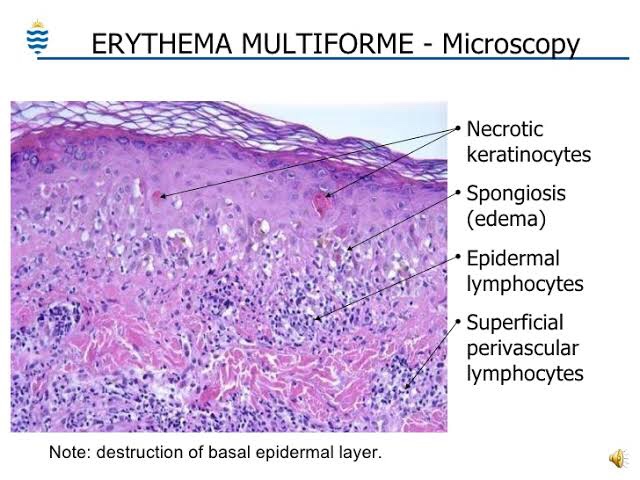
👉🏻Histopathology:
- Acanthotic mucosa
- Subepidermal non-specific vesicles with fibrous exudate
👉🏻Direct immunofluorescence is found to be the gold standard test. Deposition pattern of different types of immunoreactants differentiates the various immune-mediated diseases. Direct immunofluorescence shows presence of IgG and C3 deposits along the basement membrane zone.
👉🏻Electron Microscopy: In bullous pemphigoid (BP), the 180 kD antigen (BPAG2) was shown by immuno-EM to be a transmembrane molecule and to possess an autoantibody binding site outside the cell, suggesting a major pathogenic role for the BPAG2 in blister formation.
🔹Differential Diagnosis:
• Mucous membrane pemphigoid can be differentiated from BP by its predominant involvement of mucosal surfaces and positive Nikolsky’s sign.
• Lichen planus pemphigoides is clinically differentiated by the presence of lichen planus lesions in addition to tense blisters.
• Nikolsky’s sign is present in case of pemphigus and cicatricial pemphigoid, but not in the case of BP.
🔹 Treatment:
👉🏻Treatment is based on the degree of cutaneous and oral involvement. Mostly, topical steroid (clobetasol propionate) gives satisfactory result in case of smaller area of skin involvement, whereas larger area of skin involvement and recurrent cases are treated satisfactorily with systemic steroids and immunosuppressive agents.
👉🏻Recommended dosage for oral prednisolone is 0.3–1.25 mg/kg body weight/day, controls disease within 1–2 weeks, followed by which the dose is tapered. Dexamethasone (100 mg in 500 mL 5% dextrose i.v. over 2–3 h for three consecutive days) is the preferred steroid for pulse therapy, either administered alone or in combination with cyclophosphamide.
Other drugs for treating BP include new antibody modulators, rituximab 375mg/m2weekly over 4 weeks and omalizumab subcutaneously 300–375 mg for every 6 weeks.
👉🏻Higher doses of systemic corticosteroids seem to be associated with higher mortality rates, which led to the addition of corticosteroid-sparing agents to the treatment of BP. The most frequently used immunosuppressive agent is azathioprine (0.5–2.5 mg/kg body weight/day). Others being cyclophosphamide, methotrexate, cyclosporine A, combination tetracycline/minocycline along with nicotinamide, and more recently, mycophenolate mofetil, a DNA synthesis inhibitor, and methotrexate, a folate antagonist.
👉🏻IVIg – A dose of 1–2 g/kg for five consecutive day cycle of 0.4 g/kg/day, although a 3-day cycle may be used in cases that are nonresponsive to conventional therapy.
Dr. Mehnaz Memon🖊
References:
- http://www.jiaomr.in/article.asp?issn=0972-1363;year=2018;volume=30;issue=4;spage=432;epage=435;aulast=Aparna
- https://www.cidjournal.com/article/S0738-081X(00)00178-4/abstract
- Shafer’s Textbook of Oral Pathology, 7th edition