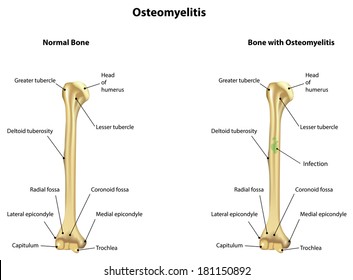
Definition: Osteomyelitis is defined as inflammation of the bone and marrow.
Classification
🔻Primary: Where bone is the primary solitary focus of disease .
🔻Secondary: Develops as a complication of any systemic infection.
Any infection (bacteria, viruses, parasites, fungi) may cause osteomyelitis but infections certain pyogenic bacteria and mycobacteria are the most common
Etiology
It is usually caused by bacteria.
• Most common pathogens are Staphylococcus species (aureus in 80-90% of the cases).
🔻Other organisms: Klebsiella, Neisseria gonorrhoeae, Haemophilus influenzae Escherichia coli, Pseudomonas, and Salmonella species
🔻Escherichia coli in patients with genitourinary tract infections or intravenous drug abusers.
Neonatal period: Haemophilus Influenzae and group B streptococci.
Patients with sickle cell disease: Salmonella infection.
• Mixed bacterial infections: It is due to direct spread or surgery or open fractures.
• In about 50%, no organisms can be isolated.
Portal entry of organisms
Causative organisms may reach the bone through the bloodstream, directly or extend from a contiguous site.
- Hematogenous spread:
• Source of organisms may be a focus of infection anywhere in the body (e.g skin pustule or infected teeth and gums, intestinal mucosa).
• Minor injuries to the mucosa (vigorous chewing of hard foods, brushing of teeth), or minor infections of the skin, release these organisms into the blood → causing temporary bacteremia → reach the bone.
•In children (5 to 15 years) and drug addicts (infected needles), it develops in the long bones.
- Direct implantation: Organisms may enter into bone by penetrating wounds, open fractures, or surgical procedures (staphylococci, streptococci, anaerobic organisms).
- Spread from adjacent (contiguous) site: e.g. infections of the feet may spread into the bone in diabetics.
Location of infection: It varies with age.
• Neonate: Metaphysis, epiphysis, or both.
•Adult: Epiphysis and subchondral regions
•Children with hematogenous spread: Metaphysis of long bones (knee, ankle, and hip).
Pathogenesis and Morphology
The sequence of events and morphological features in osteomyelitis are described together.
• Transient bacteremia: Mild injury or trauma can initiate bacteremia by organisms (eg.Staphylococcus aureus).
•Infection reaches metaphysis long bone: Because in the metaphysis capillaries form loop – which slows the blood flow provides time for bacteria to penetrate blood vessel walls and establish infective foci within the marrow.
• Inflammatory Reaction: Once in bone, the bacteria grow and induce an acute inflammatory reaction with exudates.
• Necrosis of bone: Exudate increases the pressure on the adjacent vessels and further decreases the blood supply produces bone necrosis. The necrotic areas coalesce and allow further bacterial proliferation.
•Formation of sequestrum: Bacterial infections and pus spreads into the cortex and collects beneath the periosteum and may lift the periosteum and reduce the blood supply to the affected region.
The fragment of dead necrotic piece of bone, which is embedded in the pus, is known as a sequestrum.

What is a sequestrum ?
🔻The pus penetrates the periosteum and leads to a soft-tissue abscess may penetrate the skin form a draining sinus.
Hole formed in the bone during the formation of a draining sinus is known as cloaca
🔻The sinus tract may become epithelialized and may remain open, continually draining pus, necrotic bone, and bacteria.
Involucrum
After first week, chronic inflammatory cells become more numerous and the cytokines released stimulates osteoclastic bone resorption and deposition of reactive bone in the periphery.
Reactive new bone forms a sheath around the necrotic (segment of devitalized infected bone) sequestrum. This reactive new bone formed is known as involucrum.
Variants of osteomyelitis
• Brodie abscess: It is a distinctive form of subacute pyogenic osteomyelitis.
- It appears as a small, solitary, intraosseous abscess localized to the metaphysis and is surrounded by reactive bone.
It may be due to inadequate treatment of infection by less virulent organisms.
• Sclerosing osteomyelitis of Garre – characterized by extensive newborn formation which obscures the underlying structure of the bone and typically develops in the jaw.
Complications
•Septicemia: From infection in the bone, organisms may disseminate through the blood stream and cause septicemia.
• Acute suppurative arthritis: Infection may spread through the articular surface into a joint producing suppurative arthritis may lead to destruction of the articular cartilage and permanent disability. It is more common in infants.
•Pathologic fractures.
•Squamous cell carcinoma: It may arise from the epithelialized sinus tract, rarely sarcoma of bone may develop.
• Secondary amyloidosis.
• Chronic osteomyelitis: It may develop due to delay in diagnosis, extensive bone necrosis, and inadequate therapy.
Clinical therapy
🔻 present with malaise, fever, chills , leukocytosis and throbbing pain over the affected area
🔻 Diagnosis-
Radiography- lytic focus of bone destruction
Blood cultures are positive
Biopsy and bone culture
source -textbook of pathology for dental students Harsh mohan


