The occlusal surfaces of molars, particularly the permanent first molars, are commonly affected by caries (Demirci et al., 2010). This is consistent with the findings of a study that reported over two-thirds of permanent first molars being affected by caries (Demirci et al., 2010). Additionally, the occlusal surfaces of permanent second molars also contribute significantly to caries development (Demirci et al., 2010). The high caries rates in the permanent dentition are primarily limited to the pit and fissure surfaces of molars (Demirci et al., 2010).
The pattern of caries in primary molars, specifically the maxillary incisors and first molars, is thought to be related to the eruption times of primary teeth and the acquisition of cariogenic bacteria (Xu et al., 2014). Children who develop caries before 2.5 years of age typically exhibit decay on the smooth surfaces of maxillary incisors and occlusal fissures of the first molar teeth (Xu et al., 2014).
The progression of caries lesions in primary molars is more frequent in second molars compared to first molars (Guedes et al., 2015). This is consistent with previous studies that have reported a higher probability of progression in occlusal surfaces, both in primary and permanent teeth (Guedes et al., 2015).
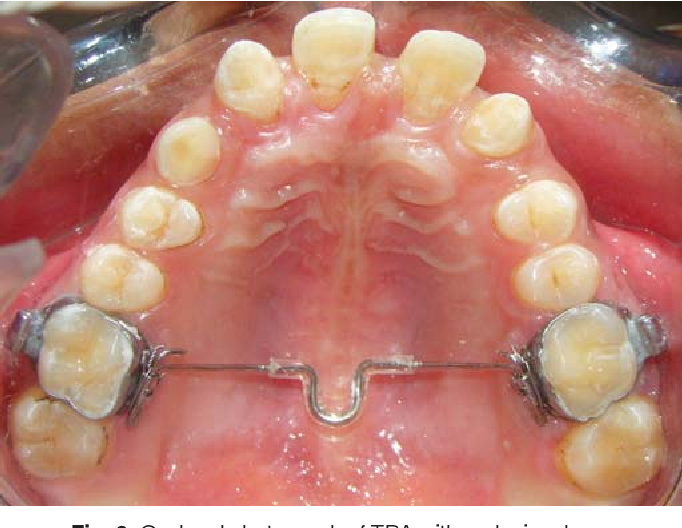
Sealants are effective in preventing and arresting pit-and-fissure occlusal caries lesions in primary and permanent molars in children and adolescents (Prabakar et al., 2018). A systematic review conducted by the American Dental Association Council on Scientific Affairs and the American Academy of Pediatric Dentistry recommended the use of pit-and-fissure sealants on the occlusal surfaces of primary and permanent molars (Prabakar et al., 2018).
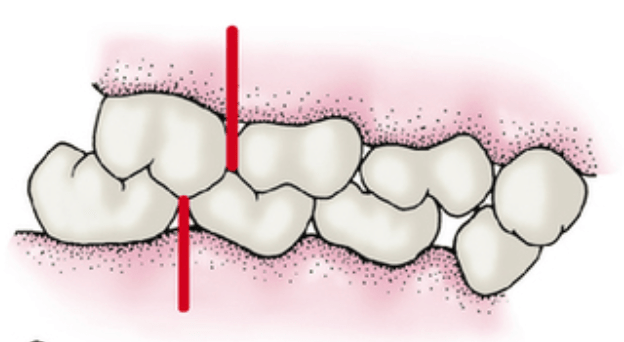
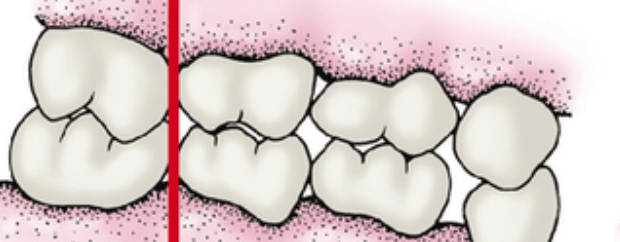
The morphology of occlusal fissures in molars plays a significant role in caries prevention (Dindar & Atay, 2022). Understanding the types of fissure morphology is important for preventing caries on the occlusal surfaces of molars and premolars (Dindar & Atay, 2022). The presence of deep occlusal pits and fissures increases the risk of plaque accumulation and subsequent decay (Alqahtani et al., 2022).
The retention of sealants on primary molars is generally lower compared to permanent molars (AL-Sultani et al., 2020). However, there is conflicting evidence regarding the effectiveness of sealants on primary molars compared to permanent molars (AL-Sultani et al., 2020). Some studies have reported that sealants are more effective in permanent molars, while others have found no significant difference in retention between primary and permanent molars (AL-Sultani et al., 2020).
The morphology of the pulp chamber in primary molars can be evaluated using spiral computed tomography (SCT) (Selvakumar et al., 2014). SCT can provide information on the distance between the central fissure and furcation, the distance between the central fissure and the floor of the pulp chamber, the height of the pulp chamber, and the distance between the floor of the pulp chamber and the furcation (Selvakumar et al., 2014).
The use of self-etching self-adhesive flowable composite for fissure sealing in primary molars has been studied (Шхагошева et al., 2021). This material has shown efficiency in sealing fissures and preventing caries in primary molars (Шхагошева et al., 2021).
The impact of occlusal tooth morphology on the penetration of fissure sealants has been investigated (Petrovic et al., 2006). The study found that the type of occlusal tooth morphology can affect the penetrating abilities of different types of sealants (Petrovic et al., 2006).
The retention of fissure sealants in primary molars can be influenced by various factors, including etching time (Duggal et al., 2009). Different etching times have been shown to affect the retention of sealants in primary molars (Duggal et al., 2009).
The efficacy of glass ionomer sealant (GIS) and fluoride varnish (NaFV) in preventing occlusal caries in primary molars has been compared (Lam et al., 2021). Both GIS and NaFV have shown effectiveness in preventing and arresting occlusal caries in primary second molars among preschool children (Lam et al., 2021).
The microtensile bond strength of bioactive pit and fissure sealants bonded to primary and permanent teeth has been evaluated (Alqahtani et al., 2022). The study found that the bond strength of sealants can vary between primary and permanent teeth (Alqahtani et al., 2022).
In conclusion, the occlusal surfaces of molars, particularly the permanent first molars, are commonly affected by caries. The pattern of caries in primary molars is related to the eruption times of primary teeth and the acquisition of cariogenic bacteria. The progression of caries lesions is more frequent in second molars compared to first molars. Sealants are effective in preventing and arresting pit-and-fissure occlusal caries lesions in primary and permanent molars. The morphology of occlusal fissures and the retention of sealants can be influenced by various factors. Understanding the occlusal morphology and evaluating the pulp chamber morphology in primary molars can provide valuable information for caries prevention and treatment.
References:
AL-Sultani, H., Al-Janabi, W., Hasan, H., Al-Murib, N., Alam, M. (2020). Clinical Evaluation Of Pit and Fissure Sealants Placed By Undergraduate Dental Students In 5-15 Years-old Children In Iraq. Pesqui. Bras. Odontopediatria Clín. Integr., (20). https://doi.org/10.1590/pboci.2020.004 Alqahtani, A., Al-Dlaigan, Y., Almahdy, A. (2022). Microtensile Bond Strength Of Bioactive Pit and Fissure Sealants Bonded To Primary And Permanent Teeth. Materials, 4(15), 1369. https://doi.org/10.3390/ma15041369 Demirci, M., Tuncer, S., Yuceokur, A. (2010). Prevalence Of Caries On Individual Tooth Surfaces and Its Distribution By Age And Gender In University Clinic Patients. Eur J Dent, 03(04), 270-279. https://doi.org/10.1055/s-0039-1697839 Dindar, M., Atay, M. (2022). Microscopic Evaluation Of Fissure Patterns Of Posterior Permanent Teeth: An In Vitro Study. Int Dent Res, 3(12), 107-111. https://doi.org/10.5577/intdentres.2022.vol12.no3.1 Duggal, M., Tahmassebi, J., Toumba, K., Mavromati, C. (2009). The Effect Of Different Etching Times On the Retention Of Fissure Sealants In Second Primary And First Permanent Molars. International Journal of Paediatric Dentistry, 2(7), 81-86. https://doi.org/10.1111/j.1365-263x.1997.tb00283.x Guedes, R., Piovesan, C., Floriano, I., Emmanuelli, B., Braga, M., Ekstrand, K., … & Mendes, F. (2015). Risk Of Initial and Moderate Caries Lesions In Primary Teeth To Progress To Dentine Cavitation: A 2-year Cohort Study. Int J Paediatr Dent, 2(26), 116-124. https://doi.org/10.1111/ipd.12166 Lam, P., Sardana, D., Luo, W., Ekambaram, M., Lee, G., Chu, C., … & Yiu, C. (2021). Glass Ionomer Sealant Versus Fluoride Varnish Application To Prevent Occlusal Caries In Primary Second Molars Among Preschool Children: a Randomized Controlled Trial. Caries Res, 4(55), 322-332. https://doi.org/10.1159/000517390 Petrovic, B., Markovic, D., Blagojevic, D. (2006). The Impact Of Occlusal Morphology On Fissure Sealant Penetration. SERBIAN DENT J, 2(53), 87-94. https://doi.org/10.2298/sgs0602087p Prabakar, J., John, J., Arumugham, I., Kumar, R., Srisakthi, D. (2018). Comparative Evaluation Of Retention, Cariostatic Effect and Discoloration Of Conventional And Hydrophilic Sealants – A Single Blinded Randomized Split Mouth Clinical Trial. Contemp Clin Dent, 6(9), 233. https://doi.org/10.4103/ccd.ccd_132_18 Selvakumar, H., Kavitha, S., Vijayakumar, R., Eapen, T., Bharathan, R. (2014). Study Of Pulp Chamber Morphology Of Primary Mandibular Molars Using Spiral Computed Tomography. The Journal of Contemporary Dental Practice, 6(15), 726-729. https://doi.org/10.5005/jp-journals-10024-1606 Xu, H., Hao, W., Zhou, Q., Wang, W., Xia, Z., Liu, C., … & Chen, F. (2014). Plaque Bacterial Microbiome Diversity In Children Younger Than 30 Months With or Without Caries Prior To Eruption Of Second Primary Molars. PLoS ONE, 2(9), e89269. https://doi.org/10.1371/journal.pone.0089269 Шхагошева, А., Маслак, Е., Фурсик, Д. (2021). The Results Of Self-etching Self-adhesive Flowable Composite Application For Primary Molars Fissure Sealing In Children. jour, 2(21), 113-117. https://doi.org/10.33925/1683-3031-2021-21-2-113-117