






Definition of syndromes are extracted from Dental pulse 13th edition.








Definition of syndromes are extracted from Dental pulse 13th edition.

Definition of syndromes are extracted from Dental pulse 13th edition.

Source: Shafer’s textbook for oral pathology
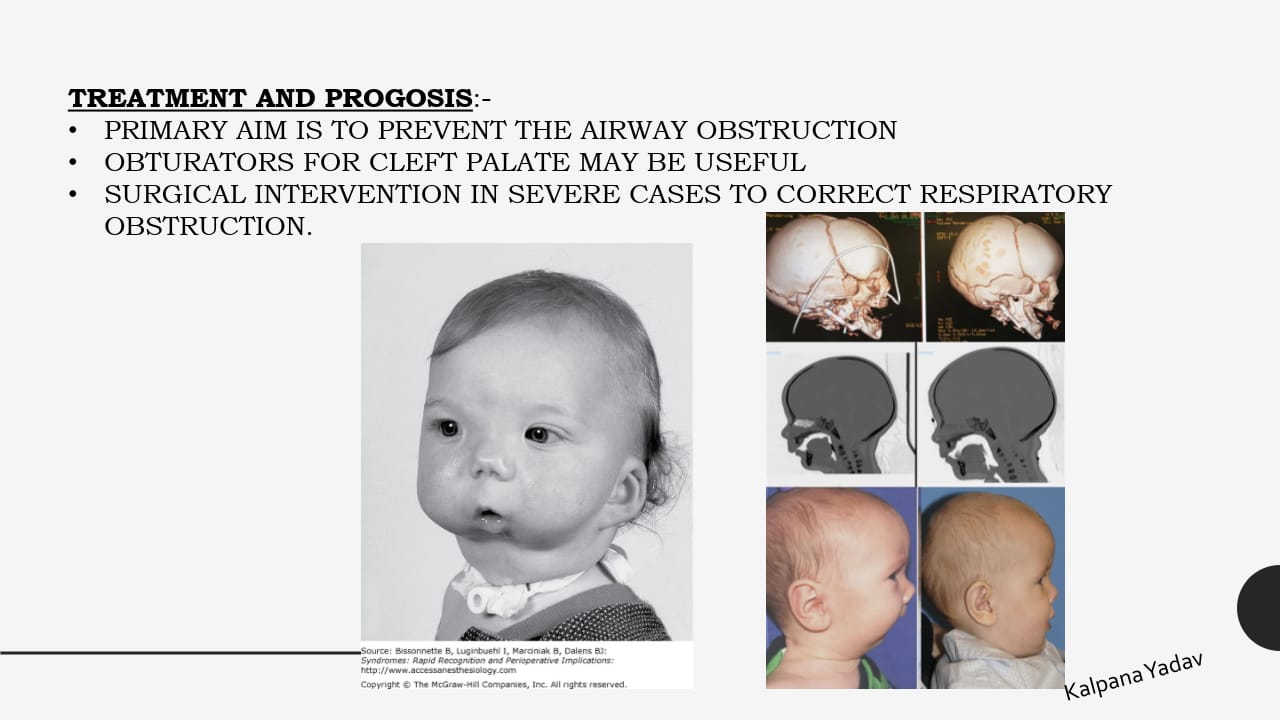
Agnathia
Micrognathia


Macrognathia


Source: Shafer’s oral pathology
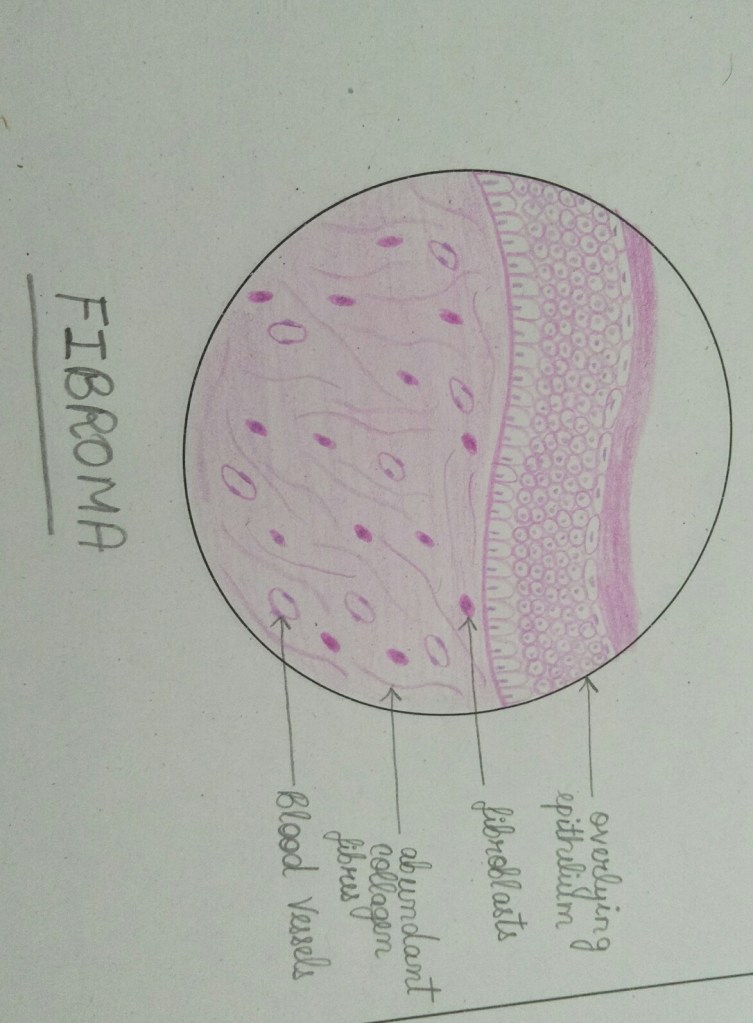
FIBROMA
LIPOMA

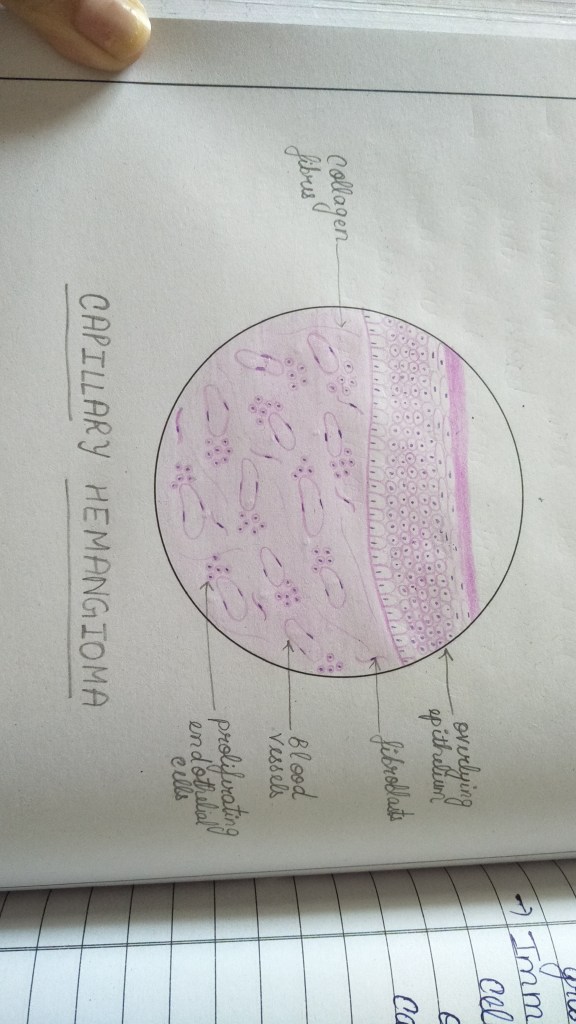
CAPILLARY HEMANGIOMA
CAVERNOUS HEMANGIOMA

LYMPHANGIOMA

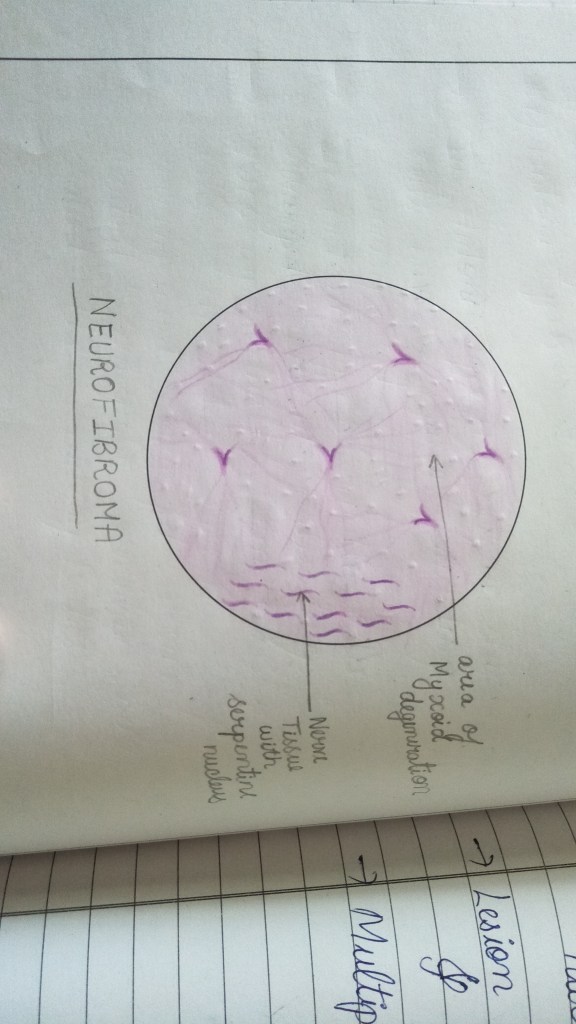
NEUROFIBROMA
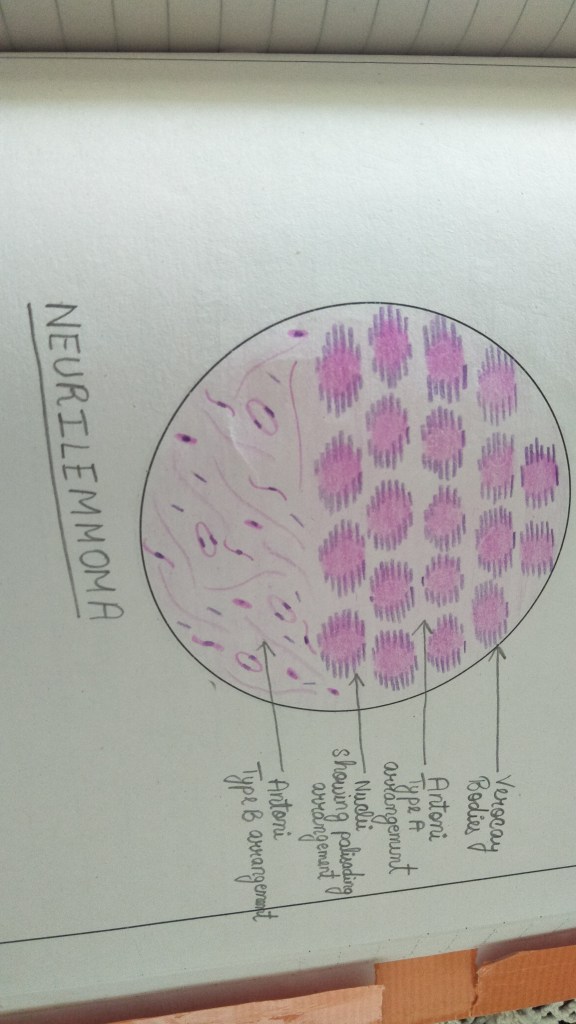
NEURILEMMOMA(SHWANNOMA)
OSTEOMA


REFERENCES- Shafer’s textbook of oral pathology 9th edition
❇️We have been hearing some terrible stories of Black Fungus and how it is spreading and causing an epidemic. This is scary. This has to be stopped and it can only be done by self care.
❇️The cause for the development of black fungus is largely attributed to the unhygienic usage of masks, yes you read that right. Each person has bacteria and virus within themselves that don’t cause any harm. There is enough evidence that the Covid recovered patients when use unhygienic masks, let the bacteria develop and grow into a fungus when it meets moisture in the mask. This gets inhaled again and thus becomes fatal.
🦷What are categorized as unhygienic masks: 1. Reusage of one time use masks 2. Sharing masks
❇️Let’s wake up now before things get worse. Let’s follow these simple steps to contain the epidemic in its initial phase.




– by Dr. Sneha poeghal BDS from Malla Reddy institute of dental sciences ,hyd.
• Swellings at the angle of Mandible include: ✍🏻👇🏻
• Branchial Cleft Cyst
(i) Benign
(ii) Malignant






• Swellings in the floor of Mouth: 👇🏻✍🏻


Differential diagnosis of swellings of the floor of the mouth or neck (Jham et al., 2007): https://www.researchgate.net/figure/Differential-diagnosis-of-swellings-of-the-floor-of-the-mouth-or-neck-Jham-et-al-2007_tbl1_287206404
• Swellings on the Palate: 👇🏻✍🏻

Differential diagnosis of palatal swellings: https://www.researchgate.net/figure/Differential-diagnosis-of-palatal-swellings_tbl1_221967546
Dentowesome|@drmehnaz🖊
Image source: Google.com
Odontogenic infection is an infection that originates within a tooth or in the closely surrounding tissues. The term is derived from Greek words “odonto” meaning “tooth” and “genic” meaning “birth”.
Odontogenic infection has plagued human kkind for as long as the human species has existed. Generally, in the orofacial region, most bacterial infections involve either a disturbance of normal flora or a displacement of the normal organisms to the site, where they are usually not seen.
Routes of odontogenic infection :
Causes of odontogenic infection :
Odontogenic infections are usually polymicrobial involving both strict anaerobes and facultative bacteria within unique ecosystems of the dental plaque and gingival crevice.
The most prevalent anaerobic bacteria include gram positive cocci such as Peptostreptococcus sp., and gram negative rods such as Bacterioids sp., Fusobacterium sp. The most prevalent aerobes are facultative gram positive such as Streptococcus mutans and Streptococcus viridans. Facultative gram negative bacilli and Staphylococcus aureus are uncommon in immunocompetent hosts but may be more important in immunocompromised patients.
Major symptoms of odontogenic infections :
Prominent physical findings include :
Imaging studies :
Complications :
Clinical manifestations of specific odontogenic orofacial space infections :
Treatment :
In normal host :
In immunocompromised host :
Source : ncbi.nlm.nih.gov
Steroids are a group of hormones produced naturally in the body.
The adrenal cortex consists of 3 zones:
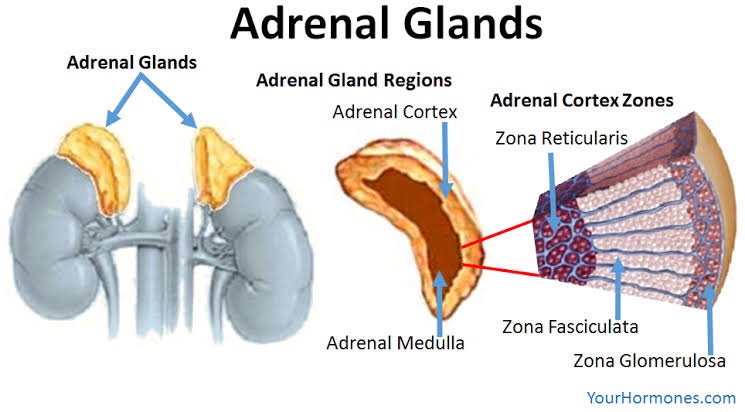
• Glucocorticoid secretion is regulated by ACTH produced in the anterior pituitary. Cortisol has a -ve feedback on ACTH production.
• In Addison diseases, Glucocorticoid secretion impaired & ACTH is ⬆️
Stress
⬇️
Release of cytokines (IL-1)
⬇️
⬆️ cortisol levels

The substrate for steroid production is cholesterol. It is mobilized from the outer to the inner mitochondrial membrane by the steroidogenic acute regulatory (StAR) protein.
• Action: Anti-allergy, anti-inflammatory
• Therapeutic Uses:
Action: Fibrinolytic,Anti-allergic, anti-inflammatory*
It causes ⬇️ fibroblastic production & deposition of collagen*
• Trade Name: CORTEF, ORABASE-HCA
• Preparation:
• Hydrocortisone acetate 25-50 mg/mL for soft tissue suspensions
• Hydrocortisone sodium phosphate: 50mg/mL IV, IM, SC
• Uses:
• Action: Anti-allergic, anti-inflammatory, immunosuppressive
• Uses:
• Trade name: DELTA-CORTEF, PRELONE
• Uses:
• Trade name: Kenolog cream
• Uses:
👉🏻Mainly used for adrenal cortical suppression
• Trade name: DECADRON
• Action: Anti-allergy, anti-inflammatory
• Uses: Lichen planus, pemphigus, Aphthae ulcer
Dr. Mehnaz Memon🖊
References: Self Notes, Image chart source: Classification of Drugs with DOC by Vikas Seth (Third Edition)
Muhad Noorman p, Final year, Team dentowesome

Reference: Shafers Textbook of maxillofacial pathology