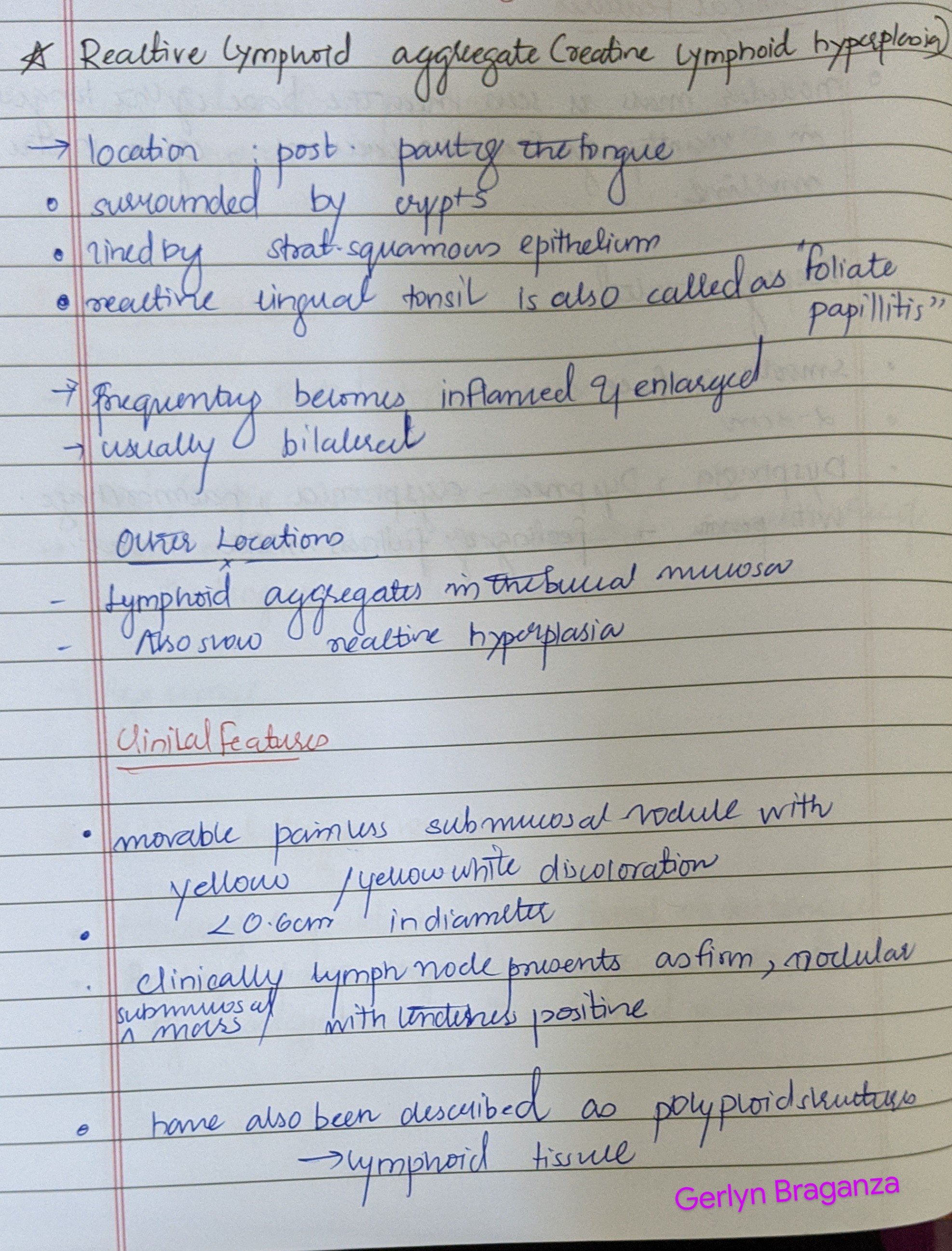
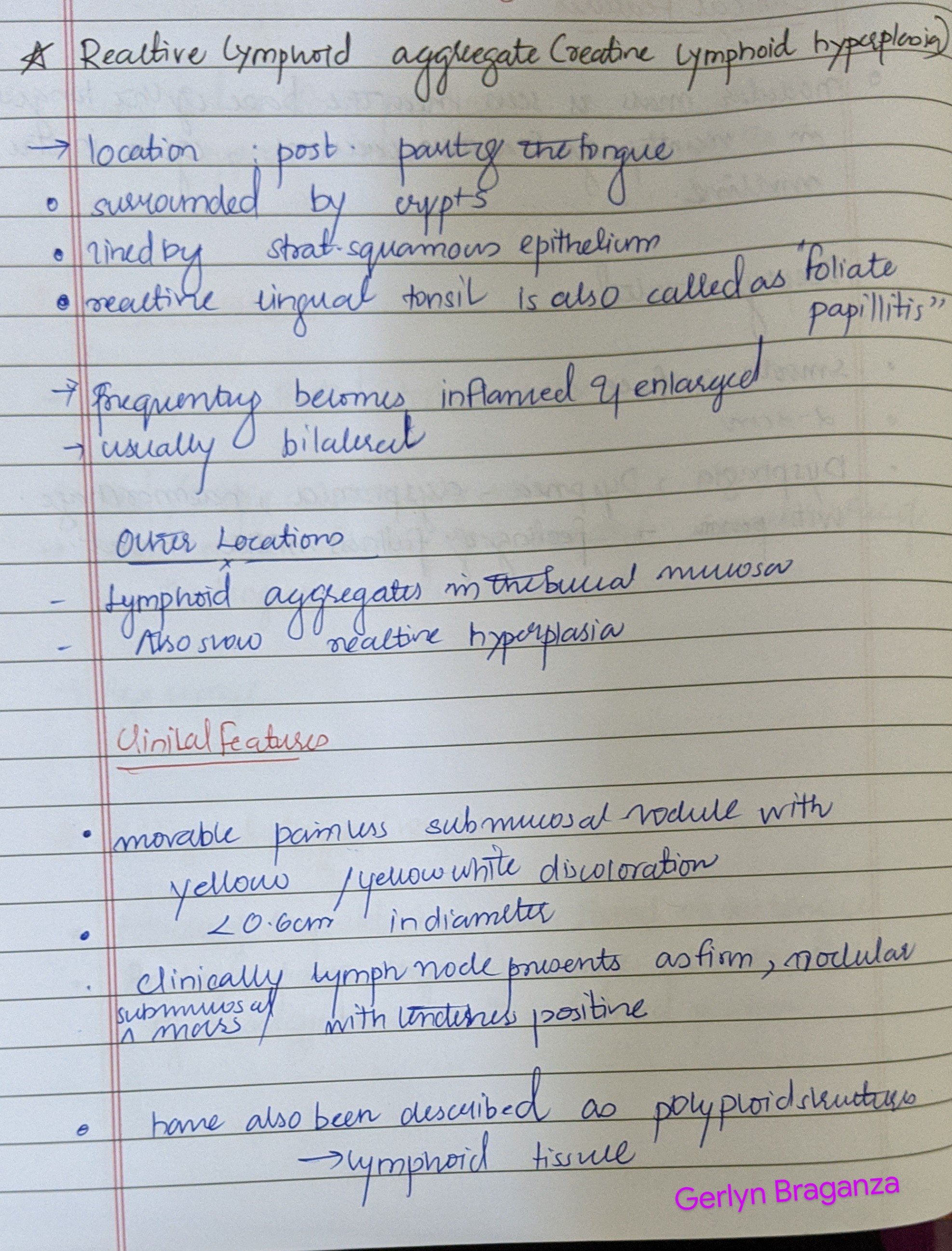
Also called as reactive lymphoid hyperplasia




Source – textbook of oral pathology Shafers and Google images
Also called as reactive lymphoid hyperplasia




Source – textbook of oral pathology Shafers and Google images
Also known as –



Source- textbook of oral pathology Shafers and Google images

Source- textbook of oral pathology Shafers and Google images



Source- textbook of oral pathology Shafers and Google images



Source- textbook of oral pathology Shafers and Google images
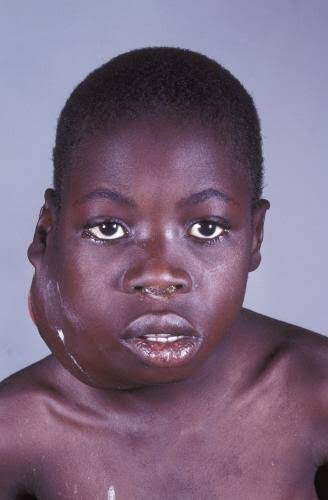
It is also called as ‘African jaw lymphoma’. It is a lymphoreticular cell malignancy. In the African form jaw involvement is 75% and in cases of the American form, abdomen involvement is more common. It is a B-cell neoplasm.
Etiology
• Epstein-Barrvirus(EBV)which also causes nasopharyn- geal carcinoma and infectious mononucleosis is considered to be the etiological factor. There are higher EBV antibody levels in patients of Burkitt’s lymphoma.
Clinical Features
Oral Manifestations
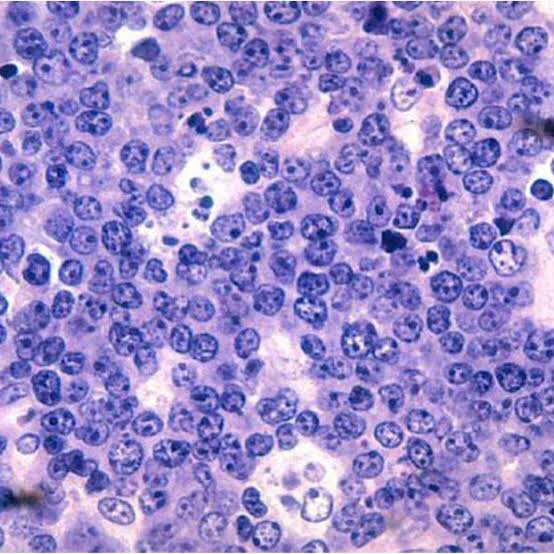
Histology
Shows characteristic starry sky appearance.

• Radiological diagnosis—moth eaten appearance is seen with loss of lamina dura around the teeth.
• Laboratorydiagnosis—monotonous sea of un differentiated monomorphic lymphoreticular cells, usually showing abundant mitotic activity. There is also hyperchro- matosis and loss of cohesiveness. Characteristic ‘starry sky’ appearance is seen.
Management
• Cytotoxicdrugs—cytotoxicdrugs like cyclophosphamide 40 mg/kg in single IV administration and repeated about 2 weeks later. Vincristine and methotrexate have been successful in some cases.
• Multiagent chemotherapy—combination of drugs such as cyclophosphamide, vincristine and methotrexate give better results than any single drug. Majority of patients show dramatic response to the therapy. The swelling regresses and the displaced teeth return to their normal position within 1 to 2 weeks.
REFERENCE- SHAFER’S TEXTBOOK OF ORAL PATHOLOGY AND ANIL GHOM TEXTBOOK OF ORAL MEDICINE
Hodgkin’s Lymphoma
Hodgkin’s disease (HD) is a lymphoid malignancy characterized by the presence of Reed-Sternberg cells of B cell origin. The disease arises usually in single nodal area and successively spreads to contiguous lymph node areas. Extranodal involvement is rare.
Types (Histological)
• Lymphocyte predominant—abundant lymphocytes, few plasma cells, occasional Reed-Sternberg cell, localized involvement of one side of diaphragm and most favorable prognosis.
• Mixed cellularity—lymphocytes, plasma cells, eosino- phils, easily identified Reed-Sternberg cell.
• Nodular sclerosis—sparse lymphocytes, stromal cells, fibrosis and numerous but bizarre Reed-Sternberg cells. It has poor prognosis.
• Lymphocyte depletion—lymphocytes, plasma cells, eosinophils with localized involvement.
ETIOLOGY
CLINICAL FEATURES
Hodgkin’s lymphoma. This high-power photomicrograph shows the characteristic Reed-Sternberg cell (arrow) of Hodgkin ‘s lymphoma, identifiedby its “owl-eye” nucleus.
Diagnosis
MANAGEMENT
Localized disease: The patients with localized disease (IA, IIA) are treated with 3 cycles of chemotherapy (ABVD-doxorubicin, bleomycin, vinblastine and dacarbazine) followed by radiotherapy of involved nodal areas.
Extensive disease: Patients with B symptoms or extensive disease receive complete course (6-8 cycles) of ABVD chemotherapy.
Long-term cure can be achieved in >90% patients with localized disease and in 50-75% patients with extensive disease.
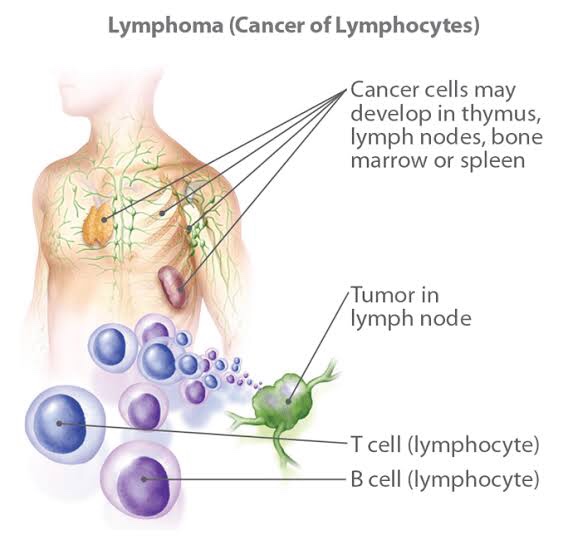
Non-Hodgkin’s Lymphoma
It is also called as ‘lymphosarcoma’. In this group, there is neoplastic proliferation of lymphoid cells, usually affecting the B-lymphocytes. Unlike Hodgkin’s lymphoma, the disease is frequently widespread at the time of diagnosis, often involving not only the lymph nodes but also bone marrow, spleen and other tissue. Early involvement of bone marrow is typical of this lymphoma.
Types (Histological)
The matted, nontender lymph node enlargement in the lateral cervical region represents a common presentation of lymphoma.
Oral manifestations
Radiographic Features
• Appearance—asthediseaseprogressessmallradiolucent foci scattered throughout the area may be seen. Subsequent radiographs of the expanding lesion will show that these small foci have coalesced to form large multilocular moth eaten radiolucency with poorly defined margins.
• Margins—lesion blends imperceptibly with adjacent normal bone, in most of the cases.
• Effect on surrounding structures—lesions may cause marked expansion of bone. Erosion and perforation of cortex may occur.
• Maxillary sinus involvement—if the lesion involves maxillary sinus, possible opacification with breached cortical walls and associated paracentral or intracentral mass.
• Teeth—cortices of unerupted tooth buds and lamina dura of adjacent teeth are lost. Teeth may be resorbed.
Diagnosis
Treatment
The disease stage is determined after clinical evaluation and investigations.
Treatment of low grade lymphoma: It depends on the stage of the disease and clinical status.
REFERENCE- SHAFER’S TEXTBOOK OF ORAL PATHOLOGY, ANIL GHOM TEXTBOOK OF ORAL MEDICINE AND GOGLE SLIDE SHARE
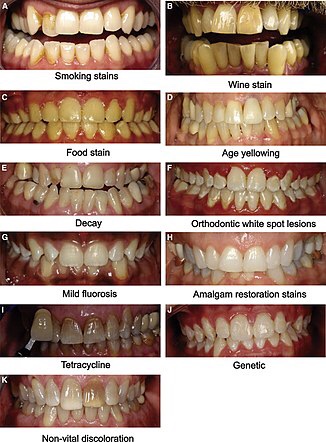
Intrinsic Stains
Pre-eruptive Causes
These are incorporated into the deeper layers of enamel and dentin during odontogenesis and alter the development and appearance of the enamel and dentin
.Alkaptonuria: Dark brown pigmentation of primary teeth is commonly seen in alkaptonuria. It is an autosomal recessive disorder resulting into complete oxidation of tyrosine and phenylalanine causing increased level of homogentisic acid.
Hematological disorders
• Erythroblastosis fetalis: It is a blood disorder of neonates due to Rh incompatibility. In this, stain does not involve teeth or portions of teeth developing after cessation of hemolysis shortly after birth. Stain is usually green, brown or bluish in color.

• Congenital porphyria: It is an inborn error of por- phyrin metabolism, characterized by overproduction of uroporphyrin. Deciduous and permanent teeth may show a red or brownish discoloration. Under ultraviolet light, teeth show red fluorescence.

• Sickle cell anemia: It is inherited blood dyscrasia characterized by increased hemolysis of red blood cells. In sickle cell anemia infrequently the stains of the teeth are similar to those of erythroblastosis fetalis, but discoloration is more severe, involves both dentitions and does not resolve with time.
Amelogenesis imperfecta: It comprises of a group of conditions, that demonstrate developmental alteration in the structure of the enamel in the absence of a systemic disorders. Amelogenesis imperfecta (AI) has been classified mainly into hypoplastic, hypocalcified and hypomaturation type.

Fluorosis: In fluorosis, staining is due to excessive fluoride uptake during development of enamel. Excess fluoride induces a metabolic change in ameloblast and the resultant enamel has a defective matrix and an irregular, hypomineralized structure



Posteruptive Causes

– Dentin deposition: Secondary and tertiary dentin deposits, pulp stones cause changes in the color of teeth.
• Functional and parafunctional changes: Tooth wear may give a darker appearance to the teeth because of loss of tooth surface and exposure of dentin which is yellower and is susceptible to color changes by absorption of oral fluids and deposition of reparative dentin.
Extrinsic Stains
Daily Acquired Stains
Plaque: Pellicle and plaque on tooth surface gives rise to yellowish appearance of teeth.
Food and beverages: Tea, coffee, red wine, curry and colas if taken in excess cause discoloration.
Tobacco use results in brown to black appearance of teeth.
Poor oral hygiene manifests as:
Swimmer’s calculus:
– It is yellow to dark brown stain present on facial andlingual surfaces of anterior teeth. It occurs due toprolonged exposure to pool water.
Gingival hemorrhage.
Chemicals
• Chlorhexidine stain: The stains produced by use of chlorhexidine are yellowish brown to brownish in nature.
Metallic stains: These are caused by metals and metallic salts introduced into oral cavity in metal containing dust inhaled by industry workers or through orally administered drugs.

Stains caused by different metals
• Copper dust—green stain
• Iron dust—brown stain
• Mercury—greenish black stain • Nickel—green stain
• Silver—black stain.
Reference- Nisha garg textbook of endosontics and Anil Ghom textbook of oral medicine

Classification of discoloration
1.Based on the Etiology of tooth discoloration
Intrinsic stains
Extrinsic stains
• Daily acquired stains
– Plaque
– Food and beverages – Tobacco use
– Poor oral hygiene
– Swimmer’s calculus
– Gingival hemorrhage.
2.Classification of extrinsic stains (Nathoo in 1997)
3.Different Types of Stains according to Color:
BLACK COLOR-
It usually results due to contact with certain metallic elements such as silver, iron and lead.It may appear as thin line running approximately 1 mm or so above the gingival margin, it may occur on both the facial and lingual surfaces of teeth.Stain is firmly attached to the surface but remains extrinsic, thus it may be removed by brush and abrasives. But, it recurs later on.

Green stain
It usually occurs as thick deposit involving the cervical one-third of facial surface of maxillary incisors of young children. It affects boys more frequently than girls.
It is associated with poor oral hygiene and decalcification is sometimes present in enamel, underlying the deposit. It occurs due to chromogenic bacteria or fungi or it may be caused by bacterial action on remnants of enamel cuticle. It is extrinsic and may be removed by simple brushing and abrasive.

Orange stain
It occurs infrequently and usually involve both facial and lingual surfaces of the incisors. It is easily removed than green stain and its cause is unknown but it is believed to be the result of chromogenic bacteria. It is associated with poor oral hygiene and removed with the help of brush and abrasives.

Brown stain
It can be seen in non-smokers and is usually lighter brown than that of tobacco and form a tenacious, but delicate film on surface of the teeth. It is usually seen more commonly on lingual surface of lower incisors and buccal surface of maxillary molar teeth. It is formed due to altered salivary mucins which have undergone change through the action of bacterial enzymes.

REFERENCE- NISHA GARG TEXTBOOK OF ENDODONTICS AND ANIL GHOM TEXTBOOK OF ORAL MEDICINE
NATAL AND NEONATAL TEETH

It is also called as ‘congenital teeth’, ‘fetal deciduous teeth’, ‘dentition proceox’ and ‘natal and neonatal teeth’. There is premature eruption of teeth or teeth like structures that are present at birth.
Natal teeth are the teeth which are present at the time of birth and neonatal teeth are the teeth which are present within 30 days after the birth.
Etiology
Hereditary—superficial position of tooth germ.
Hormonal influence—eruption accelerated by febrileincident or hormonal stimulation.
Classification
Clinical features

Management
REFERENCE- MC DONALD TEXTBOOK OF PEDODONTICS AND ANIL GHOM TEXTBOOK OF ORAL MEDICINE