













































Link to download notes:

PA radiolucencies identification made easy! Happy learning..😀📖
When formulating radiological differential diagnosis, features should be evaluated carefully, such as
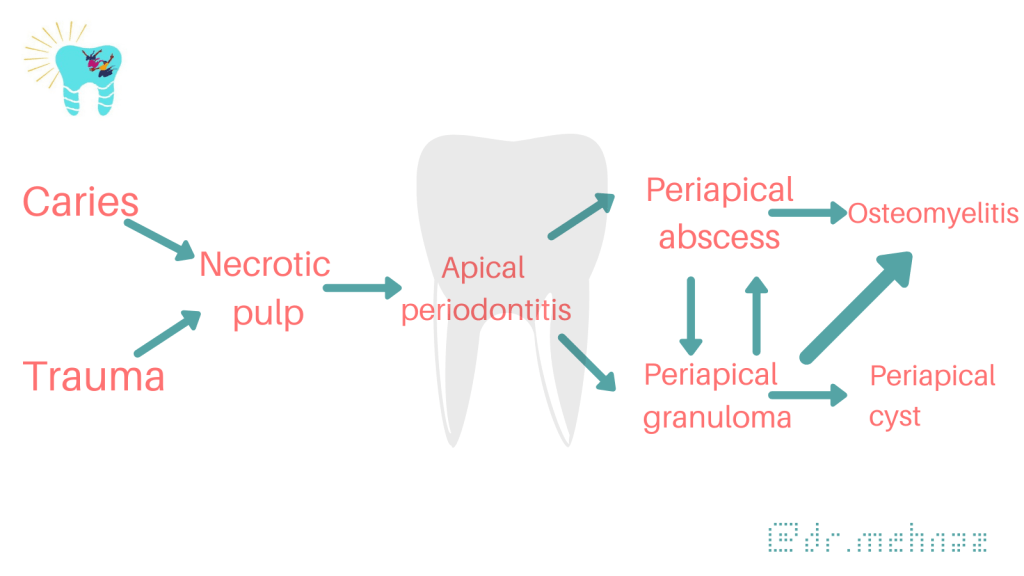
• Location: With periapical inflammatory lesions, which are pathological conditions of the pulp, the epicenter typically is located at the apex of a tooth.
• Periphery: Ill defined
• Effects on surrounding structures: Periapical lesions cause widening of PDL space at apical region of the root.

PERIAPICAL RADIOLUCENCIES
Developmental
Lateral periodontal cyst

Inflammatory Lesions
Apical periodontitis, periapical abscess


Cystic Lesions
Periapical (radicular) cyst

Odontogenic keratocyst

Glandular odontogenic cyst
Benign Tumors
Ameloblastoma

Malignant Tumors
Ameloblastic carcinoma


Dentowesome|@drmehnaz🖊
References:
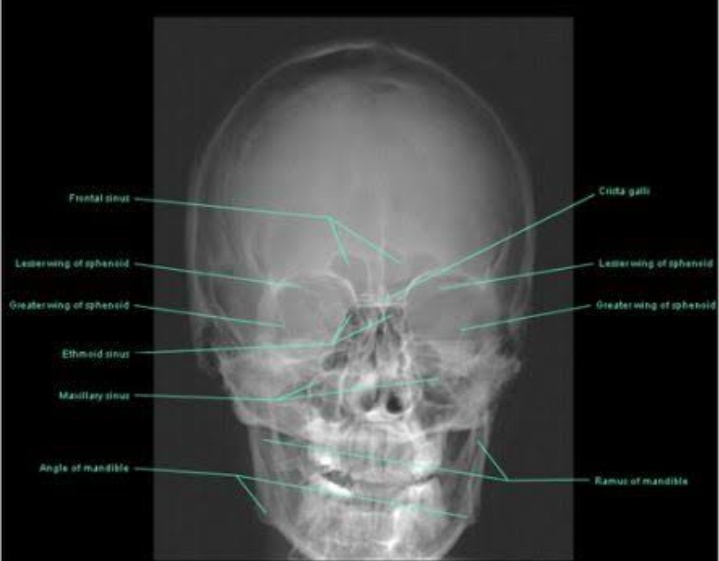
Sinus
Latin: Hollow (or) a bay
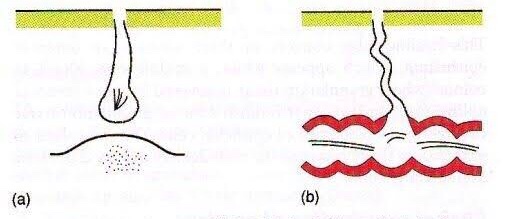
A sinus is a blind tract leading from the surface down to the tissue. There may be a cavity in the tissue which is connected to the surface through a sinus. The sinus is lined by granulation tissue which may be epithelized.
A sinus has one open draining end and the channel ends in a blind ending. An example would be a dental sinus draining from a dental abscess to either the inside of the mouth or the skin.

Fistula
Latin: flute(or) a pipe (or) a tube
It is a communicating tract between 2 epithelial surfaces commonly between hollow viscous & skin or between 2 hollow viscera. The tract is lined by granulation tissue which is subsequently epithelized. A fistula may be an abnormal communication between vessels.
An example would be from the mouth (oral cavity) to the skin surface, usually of the face or neck, and this specific type is called an orocutaneous fistula.


Fistulas and sinuses of the neck and face may be classified by cause.
Fistulas and sinuses due to developmental causes are usually present at birth.

Cysts are lumps in the skin containing fluctuant contents. They may have an opening to the skin surface.


In addition to careful history and examination, one or more of the following tests will usually be required to confirm the diagnosis and determine the cause:
Abscess
Collection of pus
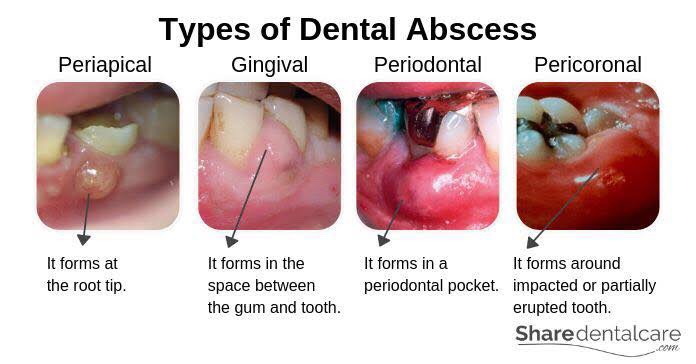
Features of acute inflammation; The four cardinal signs of inflammation are:
Diagnosis of Dental Abscess:
Dentowesome|@drmehnaz🖊
References:

A swelling is a value term that denotes only enlargement or protuberance in body due to any cause.
According to the cause a swelling may be congenital, traumatic, inflammatory, Neoplastic or miscellaneous.
Examination of a swelling should be accompanied by a complete history of the patient. Following points should be noted:
• Duration: The clinician may ask ‘when was the swelling first
noticed’? Swellings that are painful and of shorter duration are mostly inflammatory (acute), whereas those with longer duration and without pain are chronic, e.g. a chronic periapical abscess.
• Mode of onset: The clinician may ask ‘how did the swelling start’? The history of any injury or trauma or any inflammation may contribute to the diagnosis and nature of the swelling.
• Progression: The clinician should ask ‘has the lump changed in size since it was first noticed? Benign growths such as bony swellings grow in size very slowly and may remain static for a long period of time. If the swelling decreases in size, this suggests of an inflammatory lesion.
• Site of swelling: The original site where it started must be assessed.
• Other symptoms: Pain, fever, difficulty in swallowing, difficulty in respiration, disfigurement, bleeding or pus discharge are the common symptoms associated with swellings in the orofacial region.
• Recurrence of the swelling: many swellings do recur after removal of the tissue, indicating the presence of precipitating factor, e.g. ranula.

(A) Inspection

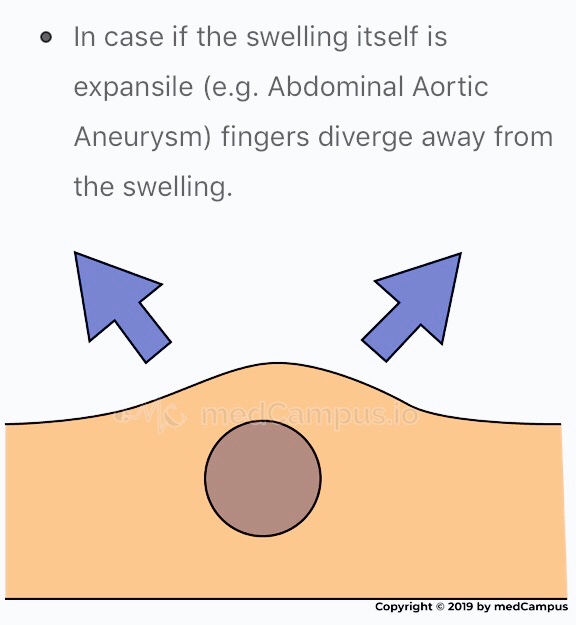

(B) Palpation

Surface: Can be👇🏻
• Smooth (cystic swellings)
• Lobular with smooth lumps (lipoma)
• Nodular (multinodular goitre)
• Matted (lymph nodes)
• Irregular (carcinoma)
Margins: Well defined/indistinct👇🏻
• Malignant growth - irregular margin
• Acute inflammatory swelling - ill defined margin
• Benign tumor - swelling slips & is indistinct
Edge👇🏻
• Well defined & regular-Benign Neoplasms
• Well defined & irregular-Malignant Neoplasms
• Ill defined & diffuse - Inflammatory swellings
Consistency: 👇🏻
• Soft - lipoma
• Cystic - Cyst or chronic abscesses
• Firm - Fibroma
• Hard - Chondroma
• Bony hard - Osteoma
• Stony hard - Carcinoma
• Variable consistency - Malignancy
An ulcer is break in continuity of epithelium, skin or mucous membrane. A proper
history must be taken in case of an ulcer:

• Mode of onset: The clinician may ask ‘how has the ulcer developed’? The patient may provide significant information about the nature and etiology of the ulcer such as any trauma or spontaneously.
• Duration: The clinician may ask ‘how long is the ulcer present here’? It determines the chronicity of the ulcer. For example, traumatic ulcers in oral cavity are acute (occurring for a short period), but if the agent persists; it may become a chronic ulcer.
• Pain: The clinician may ask ‘is the ulcer painful’? Most of the ulcers, being inflammatory in nature, produce pain. Painless ulcers usually suggest nerve diseases (such as peripheral neuritis, syphilis, etc).
• Discharge: Any blood, pus or serum discharge must be noted.
• Associated disease: Any associated generalized systemic problem may be associated with the ulcers of oral cavity (such as
tuberculosis, squamous cell carcinoma, etc).
(A) Inspection
Size & Shape:
• Tuberculous ulcer - oval with irregular border
• Varicose ulcer - vertical & oval in shape
• Carcinomatous ulcer - irregular
Number: Tuberculous, inflammatory ulcer may be more than one in number
Position:
• Arterial ulcer: Tip of the toes, dorsum of the foot
• Varicose ulcer: lower limb
• Perforating ulcers: over the sole at pressure points
• Non-healing ulcers: over the shin
• Rodent ulcer: upper part of face
Edge: An area between margin & floor. In spreading ulcer, edge is inflamed. Undermined edges destroy subcutaneous tissue faster than skin.


Floor: This is the part of the ulcer which is exposed or seen.
• Red granulation tissue - Healing ulcer
• Necrotic tissue, slough - spreading ulcer
• Pale, scanty granulation tissue - tuberculous ulcer
• Wash-leather slough - Gummatous ulcer
Discharge:
• Serous discharge - Healing ulcer
• Purulent discharge - Spreading ulcer
• Bloody discharge - Malignant ulcer
• Discharge with bony spicules - Osteomyelitis
• Greenish diacharge - Pseudomonas infection
(B) Palpation
Tenderness: Characteristic of infected ulcers and arterial ulcers.
Induration: The edge, base and the surrounding area should be examined for induration
• Maximum induration - Squamous cell carcinoma
• Minimal induration - Malignant melanoma
• Brawny induration - Abscess
• Cyanotic induration - Chronic venous congestion as in varicose ulcer
Mobility: Malignant ulcers are usually fixed, benign ulcers are not.
Bleeding: Malignant ulcer is friable like a cauliflower. On gentle palpation, it bleeds. Granulation tissue as in a healing ulcer also causes bleeding.
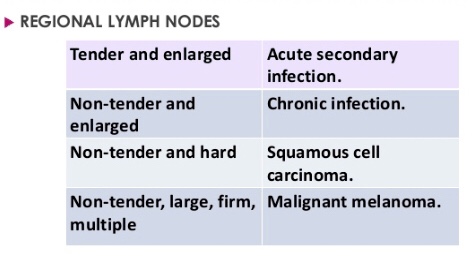
Surrounding Area:
Relevant Clinical Examination:
Dentowesome|@drmehnaz🖊
References:
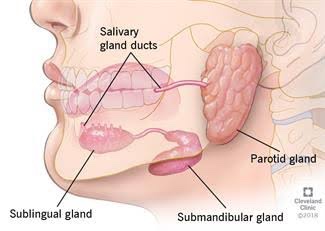
• Swellings at the angle of Mandible include: ✍🏻👇🏻
• Branchial Cleft Cyst
(i) Benign
(ii) Malignant






• Swellings in the floor of Mouth: 👇🏻✍🏻


Differential diagnosis of swellings of the floor of the mouth or neck (Jham et al., 2007): https://www.researchgate.net/figure/Differential-diagnosis-of-swellings-of-the-floor-of-the-mouth-or-neck-Jham-et-al-2007_tbl1_287206404
• Swellings on the Palate: 👇🏻✍🏻

Differential diagnosis of palatal swellings: https://www.researchgate.net/figure/Differential-diagnosis-of-palatal-swellings_tbl1_221967546
Dentowesome|@drmehnaz🖊
Image source: Google.com

Early detection and diagnosis of dental caries reduces irreversible loss of tooth structure, the treatment costs and the time needed for restoration of the teeth. Dental caries often initiates at the fissures in the occlusal surface of the tooth. Conventional examination for caries detection is primarily done using visual inspection, tactile sensation and radiographs. While these methods give satisfactory results in detection of cavitated lesions, they are usually inadequate for the detection of initial lesions. Because of these deficiencies, new detection methods have been developed to aid better diagnosis.
It is one of the most common diagnosis methods implemented by dentists. In order to make an accurate assessment, the teeth should be clean, dry and examined under a light source. In visual examination, changes in tooth structure such as; enamel dissolution, white spot lesions, discoloration, surface roughness and presence of cavitation are assessed. When illuminated, the carious tissues scatter the light and make enamel look whiter and opaque. This is due to increased porosity caused by demineralization. Similarly, when dentin undergoes demineralization, a shadow is observed under the intact enamel. When caries progress, the surface breaks down and a cavitation is formed.
The explorer and the dental floss are used for tactile examination but the use of an explorer is not preferred because:
If the explorer catches or resists removal when moderate pressure is applied, and when this is accompanied by one of the following;
Pickard, proposed the use of dental floss for the detection of caries. When there is food packing between the teeth and the floss is frayed when passed through the contact area, this might be the indication of caries.

Radiographic examination has great value in detecting caries lesions especially when they are not clinically visible. In low caries population, as a result of fluoride use, the surface of enamel does not break down, making the caries detection harder. In recent years, the incidence of such lesions has increased dramatically. According to studies, bitewing radiography has been proven to be an effective method in the detection of proximal caries and hidden caries.
Besides its advantages, radiographs also have some limitations too. For this reason, it is advisable to use clinical evaluation along with radiographic imaging. The disadvantages of radiography are as follows:
• Proximal contacts are overlapped,
• The lesion depth may appear to be increased due to angulation and this may lead to false diagnosis,
• Occlusal lesions may not be detected because of the superposition of the buccal and lingual cusps,
• The real cause of the radiolucency can’t be determined whether it is due to caries, resorption or wear,
• The superficial demineralization of the buccal and lingual surfaces may seem like proximal caries,
• Active and arrested caries can’t be distinguished in the radiographs.
• Radiographs may give false positive results due to a phenomenon called “Mach band effect”. In this perceptual phenomenon, the contrast between the dark and lighter areas has increased, resulting in a dark demarcation band. This effect causes formation of a radiolucent area in dentin enamel junction.

• Cervical burn out is another optical phenomenon where a wedge shaped radiolucent area is seen between the bone and the cemento-enamel junction. This effect is due to tissue density and the low penetration of X-rays at the cervical region.

Despite the disadvantages, radiographs are the most commonly used diagnosis tool and with the development of new techniques many of the problems are solved.

There are two layers of decalcification in carious dentin. The first one is the soft and infected layer which doesn’t have the capacity of remineralization. The second one is hard, intermediately decalcified and has the ability of remineralization. Many studies were carried out to differentiate these layers. Although there are opinions stating the benefit of caries detection dyes, there are also opinions that dyes can lead to over-reduction in the dentin.
Most clinical investigations have concluded that, caries detection dyes don’t stain bacteria but stain the less mineralized organic matrix. In a study of Demarco et al. they suggested that dye remnants that remained on the walls of the cavity may cause a decrease in the shear bond strength between the composite restorations and the enamel.
In the upcoming blog post we will learn about the Novel Methods for Caries Detection..
Happy Reading😊
References: Meandros Med Dent J 2018;19:1-8, Image source: Google
Steroids are a group of hormones produced naturally in the body.
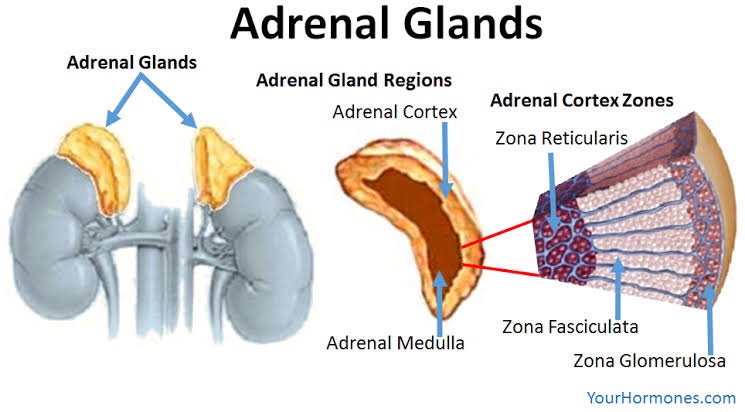
The adrenal cortex consists of 3 zones:
• Glucocorticoid secretion is regulated by ACTH produced in the anterior pituitary. Cortisol has a -ve feedback on ACTH production.
• In Addison diseases, Glucocorticoid secretion impaired & ACTH is ⬆️
Stress
⬇️
Release of cytokines (IL-1)
⬇️
⬆️ cortisol levels

The substrate for steroid production is cholesterol. It is mobilized from the outer to the inner mitochondrial membrane by the steroidogenic acute regulatory (StAR) protein.
• Action: Anti-allergy, anti-inflammatory
• Therapeutic Uses:
Action: Fibrinolytic,Anti-allergic, anti-inflammatory*
It causes ⬇️ fibroblastic production & deposition of collagen*
• Trade Name: CORTEF, ORABASE-HCA
• Preparation:
• Hydrocortisone acetate 25-50 mg/mL for soft tissue suspensions
• Hydrocortisone sodium phosphate: 50mg/mL IV, IM, SC
• Uses:
• Action: Anti-allergic, anti-inflammatory, immunosuppressive
• Uses:
• Trade name: DELTA-CORTEF, PRELONE
• Uses:
• Trade name: Kenolog cream
• Uses:
👉🏻Mainly used for adrenal cortical suppression
• Trade name: DECADRON
• Action: Anti-allergy, anti-inflammatory
• Uses: Lichen planus, pemphigus, Aphthae ulcer
Dr. Mehnaz Memon🖊
References: Self Notes, Image chart source: Classification of Drugs with DOC by Vikas Seth (Third Edition)