Sources : Shafer’s oral pathology , slideshare.com
Image source : Google images






Sources : Shafer’s oral pathology , slideshare.com
Image source : Google images

Muhad Noorman P- Dentowesome 2020
1.DENTURE STOMATITIS
Denture-induced stomatitis is a common inflammatory reaction related to the wearing of dentures usually involving Candida (yeast) species. Less common forms of denture stomatitis may be due to mechanical trauma or a contact reaction.
Predisposing factors
Denture-related stomatitis is very common, with over 50% of denture wearers affected in some populations. It is the most common clinically important condition developing in the mouth
CLINICAL FEATURE , Denture stomatitis usually does not cause any symptoms ,Some complain of burning sensations in mouth . But on examination the mouth lining in contact with the denture will be red and swollen sometimes with small red dots (petechial haemorrhages).
Treatment: regular oral hygiene, oral nystatin gargle, cleansing denture in nystatin solution, Not wearing denture at night.
2.DENTURE INDUCED FIBROUS HYPERPLASIA aka EPULIS FISSURATUM
Denture-induced fibrous hyperplasia (DIFH) is a persistent lesion caused mostly by the prolonged wear of an ill-fitting, over-extended denture. Although the condition frequently coexists with denture stomatitis, it is a distinct entity .Develops as a reactive lesion to chronic mechanical irritation produced by the flange of a poorly fitting denture.More simply, epulis fissuratum is where excess folds of firm tissue form inside the mouth, as a result of rubbing on the edge of dentures that do not fit well. It is a benign entity.
CLINICAL FEATURE: The lesion is usually painless.The usual appearance is of two excess tissue folds in alveolar vestibule/buccal sulcus, with the flange of the denture fitting in between the two folds. It may occur in either the maxillary or mandibular sulci,although the latter is more usual.Anterior locations are more common than posterior. Less commonly there may be a single fold, and the lesion may appear on the lingual surface of the mandibular alveolar ridge.
Surgically excised, reconstruction of denture, denture rebasing can be done
3. DENTURE INDUCED ULCER
Traumatic ulcers caused by dentures with overextended or unbalanced occlusion are seen in about 5% of denture wearers.Overextention of flanges,sequestration of bony spicules, illfitting, sharp boders are cause of Traumatic ulcer.
CLINICAL FEATURE: Superficial, Painful, shallow ulceration often with erythematous halo and greyish membrane covering the ulcer.
Symptomatic relief by topical analgesic,steroid oinments and repair of denture.
4. INFLAMMATORY PAPILLARY HYPERPLASIA OF PALATE
Inflammatory papillary hyperplasia (IPH) is a benign lesion of the palatal mucosa. It is usually found in denture-wearers but also has been reported in patients without a history of use of a maxillary prosthesis use.The lesion almost exclusively involves the hard palate
CLINICAL FEATURES:
Inflammatory papillary hyperplasia is usually asymptomatic. It presents as a cluster of individual papules or nodules that may be erythematous, somewhat translucent, or normal in surface coloration. Mucosa is erythematous and has a pebbly or papillary surface. Many cases are associated with denture stomatitis.
Often the entire vault of the hard palate is involved .Has a female prediliction.
This may be aided by use of topical antibiotic or antifungal therapies. Small lesions are also typically treated with mouthrinses such as chlorhexidine mouthrinse at 0.12% or antifungal mouthrinse/ gels. Larger lesions recquired surgical excision.
References: Neville Textbook of Oral pathology.
Shafers textbook of pathology. Cover photo image: Internet
Muhad Noorman P- Dentowesome 2020
During impacted teeth extraction process,Surgical managment of facial fractures with high speed rotary instruments like airotor, blowing of compressed air into root canal , airotor in middle face fractures with use of air-pushing machine such as airotor or even an air syringe, Due to air leakage inside the tissues can cause the phenomenon of confined air within tissues called Cervicofacial Emphysema and is the result of air trapping, so use the micromotor handpiece instead of the airotor, because it is a dangerous condition._The treatment is only to reassure the patient that it will go away after 3-4 days. However rarely can cause Venous Air Embolism, mediastenal emphysema and rarely pneumothorax.
Clinically presented as unilateral swelling of face/neck with or without dysphagia resembling Angioedoema,however crepitus on palpation is a positive diagnostic feautre.
Another type is PNEUMOPAROTID,entrapment of air in parotid duct either accidental or by profession in trumphet blowing artist etc.. presenting with painful swelling in face over parotid region with froathy saliva.and ctepitus on palpation.
References: Shafer’s Textbook of Oral Pathology
Muhad Noorman P – Dentowesome 2020
Papillon–Lefèvre syndrome (PLS) is a rare autosomal recessive disorder, characterized by diffuse palmoplantar keratoderma (hyperkeratosis) and precocious aggressive periodontitis, leading to premature loss of deciduous and permanent dentition at a very young age. Various etiopathogenic factors are associated with the syndrome, like immunologic alterations, genetic mutations, and the role of bacteria. Dentists play a significant role in the diagnosis and management of PLS as there are characteristic manifestations like periodontal destruction at an early age and an early eruption of permanent teeth. Here, we are presenting an elaborate review of PLS, its etiopathogenesis, clinical presentation, and management options.
Genetic studies of patients with Papillon-Lefèvre syndrome have mapped the major gene locus to chromosome 11q14-q21 and revealed mutation and loss of function of the cathepsin C gene. This gene is important in the structural growth and development of the skin and is critical for appropriate immune response of myeloid and lymphoid cells. Researchers believe that the loss of appropriate function of the cathepsin C gene results in an altered immune response to infection. In addition, the altered gene may affect the integrity of the junctional epithelium surrounding the tooth.
A closely related disease, Haim-Munk syndrome, also exhibits palmoplantar keratosis, progressive periodontal disease, recurrent skin infections, and several skeletal malformations. In this syndrome, the skin manifestations are more severe and the periodontal disease is milder. Studies have demonstrated that Haim-Munk syndrome and many examples of prepubertal periodontitis also exhibit mutation of the cathepsin C gene and represent allelic variants of the mutated gene responsible for Papillon-Lefèvre syndrome.


References: Shafer’s Textbook of Oral 9th edition
Photo credits: Dr Karthikeyan,PG final year Periodontics,Saveetha dental College, Chennai





REGARDS,
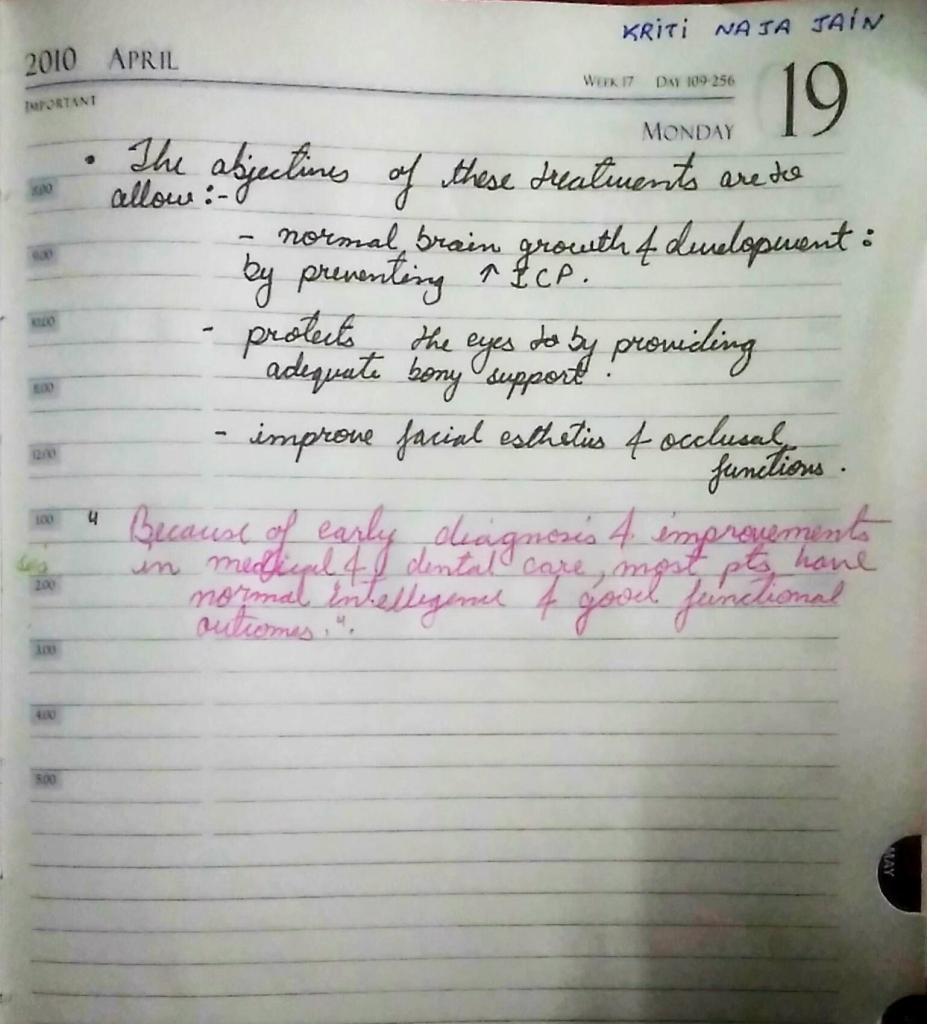
Kriti Naja Jain 🙂
References:-
White & Pharow 7th e

source – Nancy 13th edition
➡️ The periapical expressions of pathologic Amelogenesis are hypoplasia, which is manifested by pitting, furrowing or even total absence of enamel & hypocalcification in the form of opaque or chalky areas on normally contoured enamel surfaces.
➡️ It is caused by systemic, local or hereditary factors
➡️ An example of systemic type of calcification of the enamel is so called Mottled Enamel
➡️ High flouride content in water – deficiency to calcify
➡️ The discoloration of the teeth from administration of tetracyclins during childhood is very common clinical problem
➡️ Dentin sensitivity of pain is exlained by hydrodynamic theory, the alteration of the fluid & cellular contents ending in contact with these cells.
➡️ Erosion of peritubular dentin & smear plug removal accounts for dentin hypersensitivity caused by agents like acidic soft drinks.
➡️ The rapid penetration & spread of caries in the dentin is the result of the tubule system in the dentin
➡️ Electron microscope of carious dentin show regions of massive bacterial invasion of dentinal tubules.
➡️ Smear layer consist of cut dentin surface which occludes the tubules & reduces permeability. Also prevents adhesion of restorative materials to dentin. Therefore this layer is removed by etching.
➡️ Cementum is more resistant to resorption than bone. It is for this reason orthodontic tooth movement is made possible.
➡️ Cementum resorption can occur after trauma or excessive occlusal forces. After resorption has ceased the damage usually is repaired either by formation of acellular/cellular cementum or alternate formation of both.
➡️ In most cases of repair there is tendency to re-establish the former outline of the root surface. This is called anatomic repair.
➡️ It is only a thin layer of cementum is deposited on the surface of resorption, the root outline is not reconstructed & a baylike recess remains. This is termed functional repair.
➡️ Hypercementosis – secondary to periapical infammation or extensive occlusal stress. Extraction of such tooth may necessitate the removal of bone.
Source: Internet
Dentowesome 2020 @dr.mehnaz

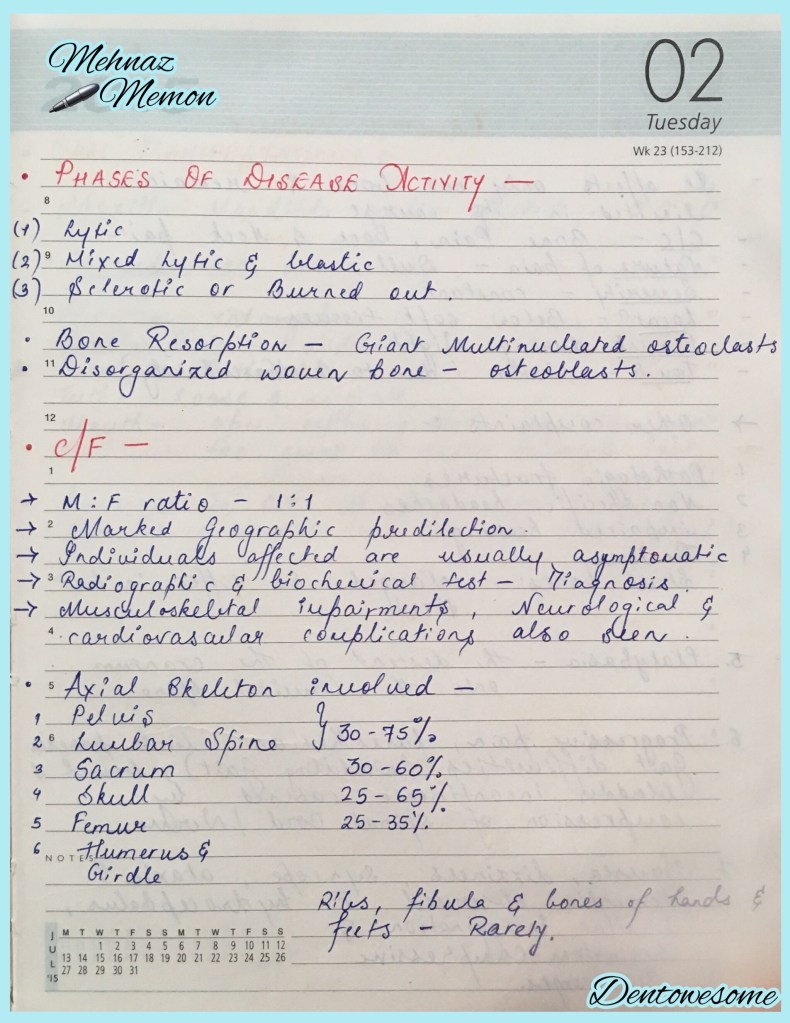




References: Shafer’s Textbook of Oral Pathology 7th Edition
Dr. Mehnaz Memon🖊
SOURCE – GHOMS TEXTBOOK
SOURCE – GHOMS TEXTBOOK