

Source White Pharaoh textbook


Source White Pharaoh textbook
Name suggested by Willis.
Most common neoplasm of salivary gland tumor.
Benign neoplasm- consisting of cells exhibiting the
ability to differentiate to epithelial (ductal and
nonductal) cells and mesenchymal (chondroid,
myxoid, osseous) cells.
Other names:
Salivary gland tumor origin: EPITHELIAL
Shows cytogenic abnormalities in chomosomes- 12q13-15.
Putative pleomorphic adenoma gene(PLAG1) has been
mapped to chromosomes 8q12
Histogenesis:-
CLINICAL FEATURES:-
Most common tumor.
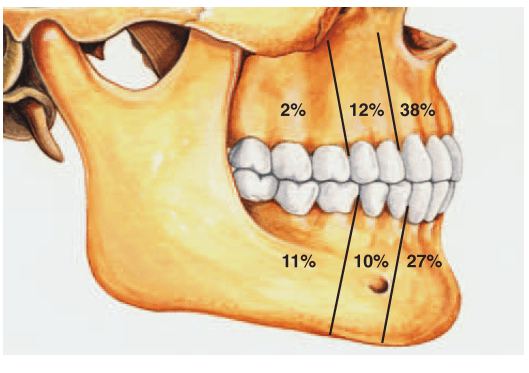
Rate of occurance: 60-70%- parotid glands
40-60%- submandibular glands
40-70%- minor salivary glands
seldomly- sublingual glands
Age: 30-50 years
Sex: female> male – 3:1 – 4:1
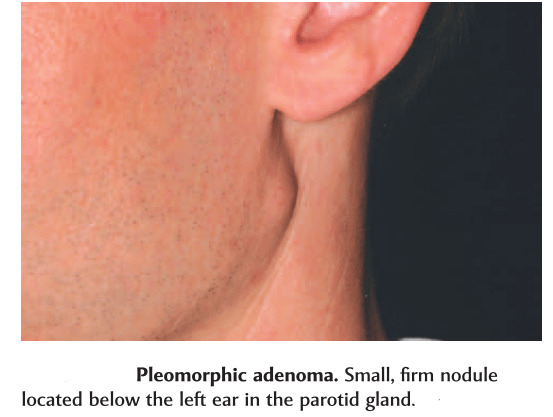
In parotid- presents in the lower lobe of the superior lobe
as a mass over the angle of the mandible, below and infront
of the ear.
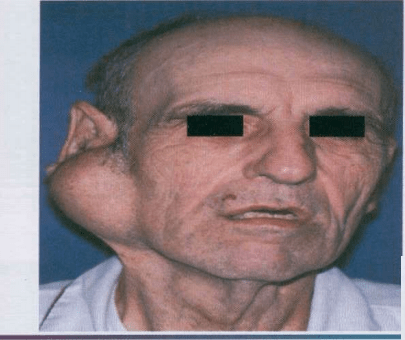
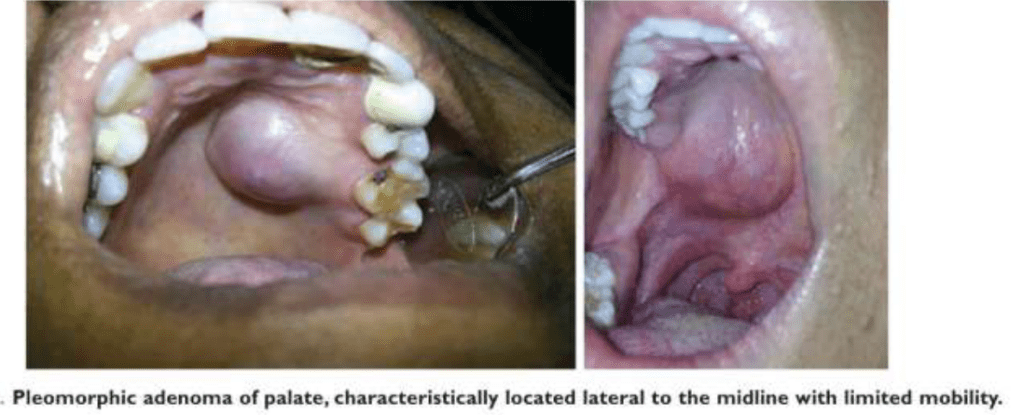
Clinical presentation: painless, slow growing, firm
mass, initially small in size and begins to increase in
size.
Initially movable but with continued growth become
more nodular and less movable.
Recurrent tumor- multinodular, fixed on palpation.
Palate – intraorally common site.
Seldom ulcerated- unless secondarily traumatized.
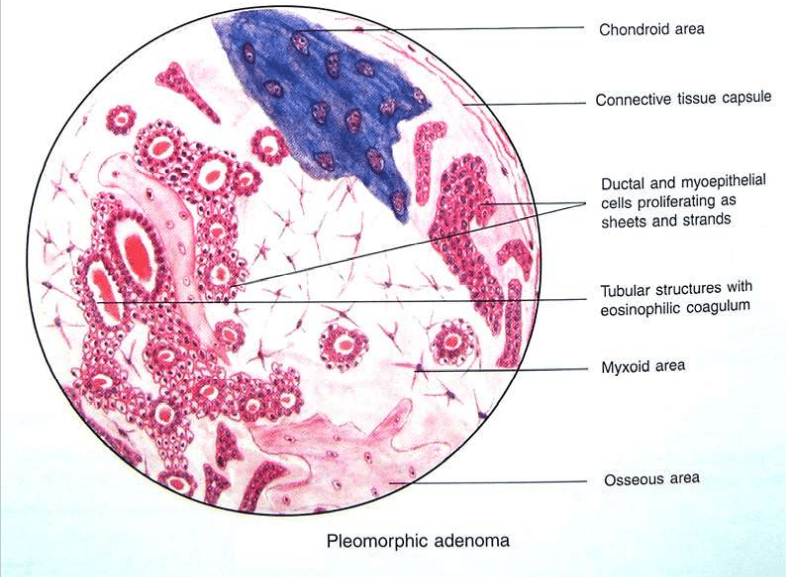
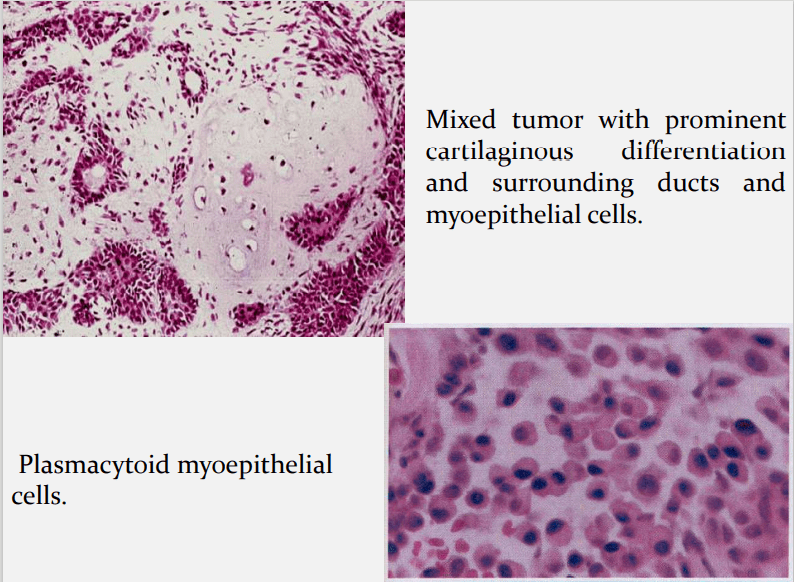
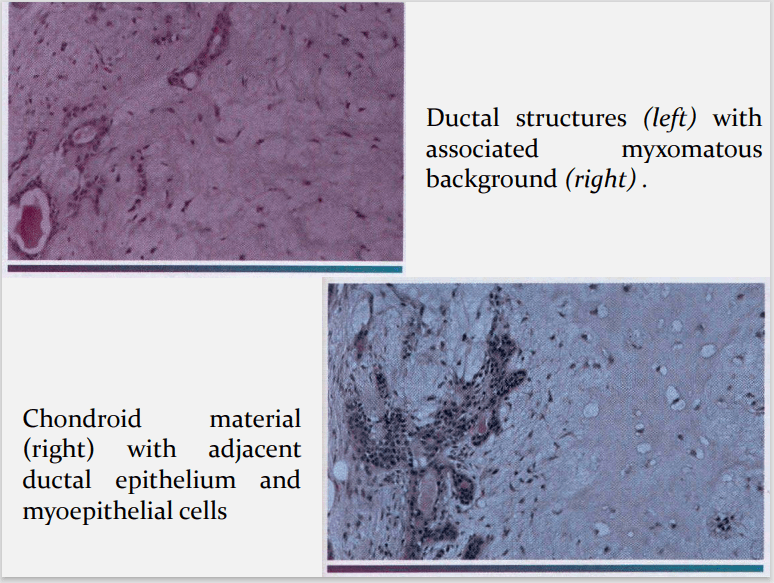
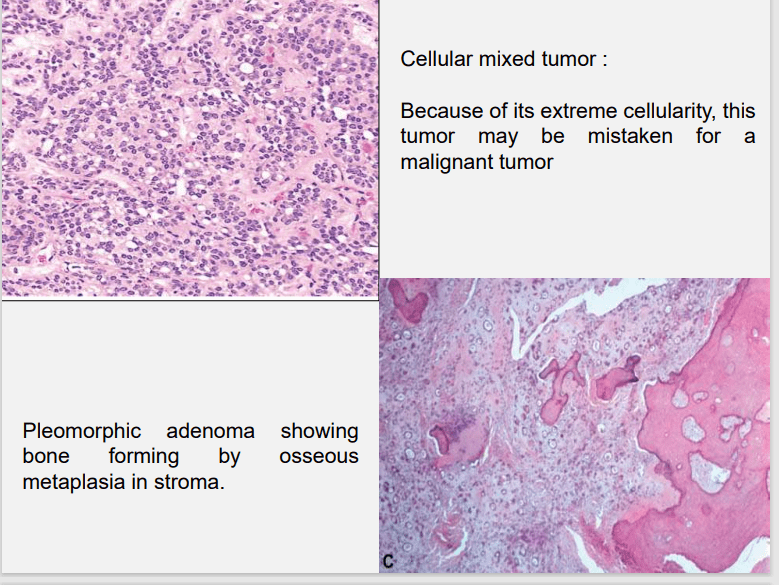
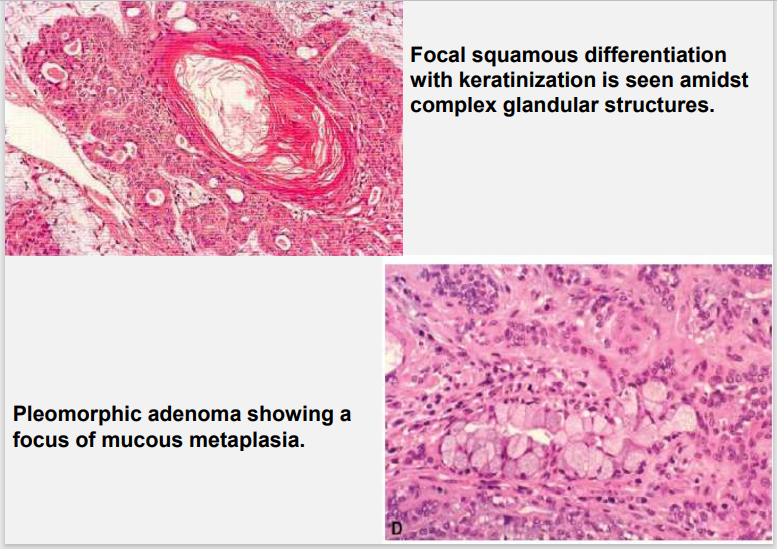
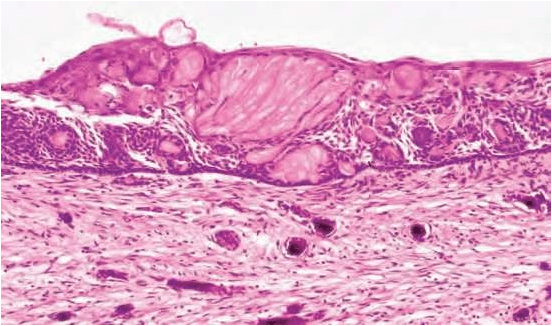
HISTOPATHOLOGY:-
HALLMARK: Morphologic Diversity.
Charecterized by- Variable, Diverse, Structural & histologic
patterns.
It demonstrate glandular epithelium and mesenchyme like
tissue and the proportion of each component varies widely.
Typically a well-circumscribed encapsulated tumor
The epithelium often forms ducts and cystic structures or may
occur as islands or sheets of cells , anastomosing cords and foci
of Keratinizing squamous cells and spindle cells .
Myoepithelial cells are major component of PA.
Have variable morphology- sometimes appearing as
angular or spindled, some with eccentric nucleus
resembling plasma cells.
Are responsible for characteristic mesenchyme like
changes.
Vacuolar degeneration of myoepithelial cells can produce a
chondroid appearance.
the stroma exhibits areas of an eosinophilic hyalinized change,
fat or osteoid also is seen.
DIFFIRENTIAL DIAGNOSIS:-
Polymorphous low grade adenocarcinoma, PLGA
Adenoid cystic carcinoma, AdCC
Epithelial myoepithelial carcinoma, EMC
Squamous cell carcinoma, SCC
Mucoepidermoid carcinoma, MEC
TREATMENT:-
Surgical excision
Superficial parotidectomy with preservation of the facial nerve
Local enucleation should be avoided – resulting in seeding of
the tumor bed.
Deep lobe of the parotid- total parotidectomy is usually
necessary also with preservation of the facial nerve.
Submandibular tumors – Total removal of the gland with the
tumor.
Malignant degeneration is a potential complication, resulting in
a carcinoma ex pleomorphic adenoma.
The risk of malignant transformation is probably small, but it
may occur in as many as 5% of all cases.
REFERENCES:-
1.Shafers- 8e
2.Nevill’s-3rd e
3.Maji Jose
4.GOOGLE Images
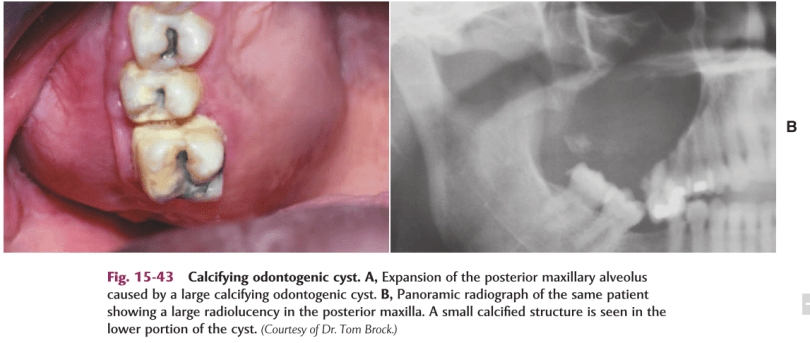
DEF:-Calcifying odontogenic cyst (COC), previously known as Gorlin cyst, is a rare, well-circumscribed, solid or cystic lesion derived from odontogenic epithelium that resembles follicular ameloblastoma but contains ‘ghost cells’ and spherical calcifications.
Other Names:-
1.Keratinizing and/or Calcifying Epithelial Odontogenic Cyst,
2.Gorlin Cyst
3.Cystic Keratinizing Tumour
4.Dentinogenic Ghost Cell Tumour
5.Odontogenic ghost cell cyst

*Radiograph of a calcifying odontogenic cyst with well-demarcated margins extending from the right to the left premolar regions of the mandible. Numerous calcifications are present, some suggestive of small denticles.
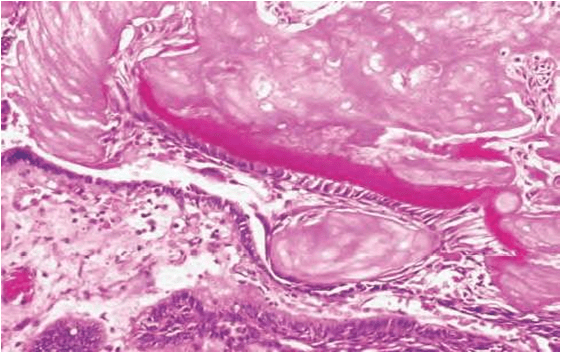
defined cell boundaries.
5.Some times many cells may fuse.
6.They represent abnormal keratinization and frequently calcify.
7.Tubular dentinoid and even complex odontome may be found in connective tissue wall close to epithelial lining.
Based on radiographic appearance, following lesions must be included in the provisional diagnosis –
References :-
1.Shafers- 8e
2.Neville -3e
3.Google-Slideshare
A continuation of the previous post on syndromes and easy short forms to remember the key features. Hope you find it helpful. Sources: Shafers textbook of oral pathology,www.rxpg.com,instagram–@_dentistars_,@dental_exams,www.medinaz.com

• Occlusal restoration—some suggested that occlusal restoration may lead to weakening of tooth ability to resist the stresses of occlusion leading to abfraction.
• Predisposing factors—factors, such as erosion and abrasion may play a significant role in tooth tissue loss.
Clinical features
REFERENCE- ANIL GHOM TEXTBOOK OF ORAL MEDICINE [2nd ed]
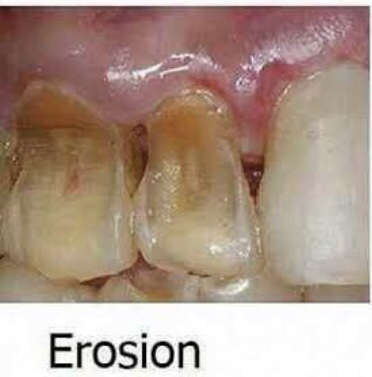
It is the loss of tooth substance by chemical process that does not involve known bacterial action. Dissolution of mineralized tooth structure occurs due to contact with acids. Erosion is a chemical process in which the tooth surface is removed in the absence of plaque.
Types (depending upon etiology)
• Sites—It occurs most frequently on labial and buccal surfaces of teeth; some times, may occur on proximal surfaces of teeth. Usually confined to gingival thirds of labial surface of anterior teeth. Erosion may involve several teeth of dentition. From extrinsic source, it causes erosion on labial and buccal surface and from intrinsic source, it causes erosion on lingual or palatal source.
REFERENCE- ANIL GHOM TEXTBOOK OF ORAL MEDICINE [2nd ed]
Abrasion is the pathological wearing away of tooth substance through some abnormal mechanical process. Abrasion usually occurs on the facial surface of the crown and the exposed root surfaces of teeth, but under certain circumstances it may be seen elsewhere such as on incisal or on proximal surfaces.

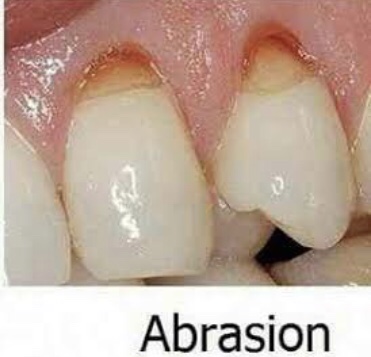
• Mechanism—it occurs due to back and forth movement of brush with heavy pressure causing bristles to assume wedge shaped arrangement between crown and root.
• Appearance—in horizontal brushing there is usually a ‘V’ shaped or ‘wedge’ shaped ditch on the root at cementoenamel junction . It is limited coronally by enamel.
• Symptoms—patient develops sensitivity as dentin becomes exposed.
• Signs—the angle formed in the depth of the lesion as well as that of enamel edge is a sharp one. Cervical lesions caused purely by abrasion have sharply defined margins and a smooth, hard surface. The lesion may become more rounded and shallow, if there is an element of erosion present.
• Dentinal features—exposed dentin appears highly polished Exposure of dentinal tubules and consequent irritation of the odontoblastic processes stimulates secondary dentin formation which is sufficient to protect the pulp from clinical exposure.
Dental floss or tooth pick injury
• Site—Cervical portion of proximal surfaces ,just above the gingival margin, is affected. Grooves on distal surface are deeper than on mesial surface
Radiographic features
Tooth brush injury
• Modified teeth cleaning habits—modification of teeth cleaning habits will be indicated.
• Removal of cause—elimination of causative agent should be carried out.
• Restoration—restoration should be done for esthetics purpose and to prevent further tooth wear.
REFERENCE- ANIL GHOM TEXTBOOK OF ORAL MEDICINE [2nd ed]
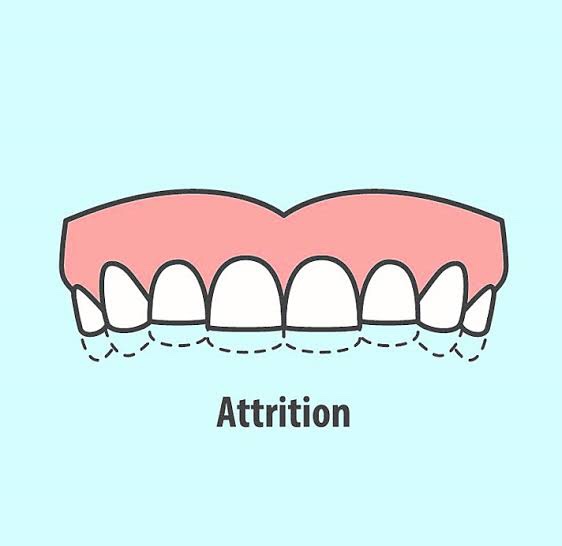

Types
• Physiological attrition—attrition which occurs due to normal aging process, due to mastication.
• Pathological attrition—it occurs due to certain abnor- malities in occlusion, chewing pattern or due to some structural defects in teeth.
Etiological factors for pathological attrition
• Abnormal occlusion
• Developmental—malocclusion and crowning of teeth, may lead to traumatic contact during chewing, which may lead to more tooth wear.
• Acquired—due to extraction of teeth. Extraction causes increased occlusal load on the remaining teeth, as the chewing force for the individual remains constant.
• Premature contact in case of edge-to-edge contact,pathological attrition can also occur.
• Abnormal chewing habits parafunctional chewing habit like bruxism and chronic persistent chewing of coarse and abrasive food or other substances like tobacco.
• Occupation in certain occupations, workers are exposed to an atmosphere of abrasive dust and cannot avoid it getting into mouth.
• Structural defect in defects like amelogenesis imperfecta and dentinogenesis imperfecta, hardness of enamel and dentin is reduced and such teeth become more prone to attrition.
Clinical features
• Sex—men usually exhibit more severe attrition than women due to greater masticatory forces.
• Sites—it may be seen in deciduous as well as permanent dentition. It occurs only on occlusal, incisal and proximal surfaces of teeth. Severe attrition is seldomly seen in primary teeth, as they are not retained for any great period. Palabal cusps of maxillary teeth and buccal cusps of mandibular posterior teeth show most wear.
• Appearance – the first clinical manifestation of attrition is the appearance of small polished facet on a cusp tip or ridge and slight flattening of an incisal edge.
Physiologic attrition
• Pathologicalattrition
Severe tooth loss—in pathological attrition severe tooth loss is seen .
Dentoalveolar compensation—if attrition affecting the occlusal surfaces of teeth has occurred, then reduction in occlusal face height (vertical dimension of occlusion) and increase in the freeway space could be anticipated. This may be further complicated by forward posturing of mandible. It is often observed, however, that despite overall tooth surface loss, the freeway space and the resting facial height appear to remain unaltered primarily because of dentoalveolar compensation. This is important with respect to patient assessment. If restoration of worn teeth is being planned then the extent of dentoalveolar compen- sation would appear to determine the dentist’s strategy; defining the need to carry out measures such as crown lengthening, to ensure the same vertical dimension of occlusion and freeway space.
Radiographic features
• Crown—smoothwearingofincisalandocclusalsurfaces of involved teeth is evident by shortened crown image
• Pulp—sclerosisofpulpchamberandcanalsisseendue to deposition of secondary dentin which narrows the pulp canals.
• Periodontal ligament—widening of periodontal ligament space and hypercementosis.
• Alveolar bone—some loss of alveolar bone.

Management
REFERENCE- ANIL GHOM TEXTBOOK OF ORAL MEDICINE [2nd ed]
Source White Pharaoh textbook
Source White Pharaoh textbook