- Behçets disease (BD) was initially described by the Turkish dermatologist Hulusi Behçet as a triad of symptoms including
1. Recurring oral ulcers,
2.Recurring genital ulcers, and
3.Eye involvement.
ETIOLOGY
- The cause of BD is unknown,
- but immune dysregulation,
- including circulating immune complexes,
- autoimmunity, cytokines, and
- heat shock proteins,
- major factor in the pathogenesis of BD.
CLINICAL MANIFESTATIONS
- Highest incidence is in young adults between the ages of 25 and 40.
- The most common site of involvement is oral mucosa.
- The genital area is the second most common site of involvement and presents as ulcers
- The eye lesions consist of uveitis, retinal vasculitis, vascular occlusion, optic atrophy, and conjunctivitis.
- Blindness is a common complication of the disease, and periodic evaluation by an ophthalmologist is necessary.
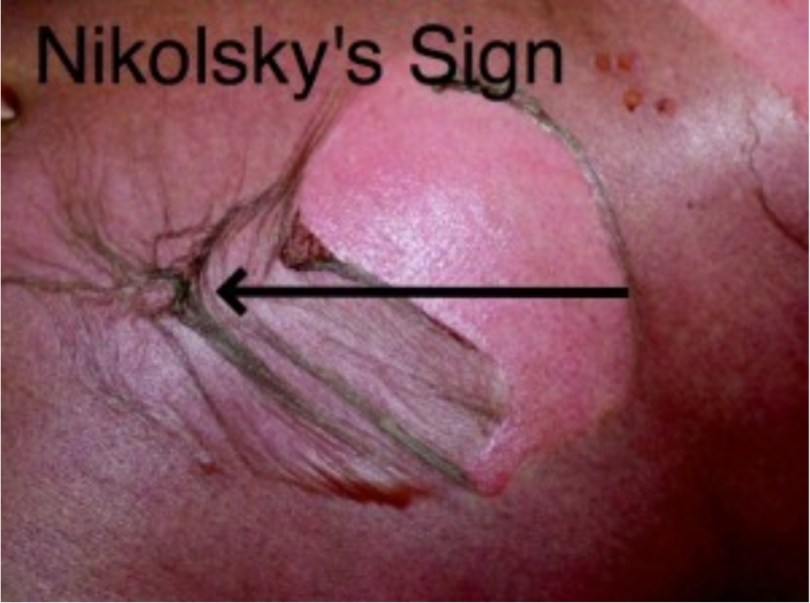
- Positive pathergy is defined as an inflammatory reaction forming within 24 hours of a needle puncture scratch, or saline injection.
- A positive pathergy test, which is performed by placing a 20 gauge needle 5 mm into the skin of the forearm. The test is positive if an indurated papule or pustule greater than 2 mm in diameter forms within 48 hours.
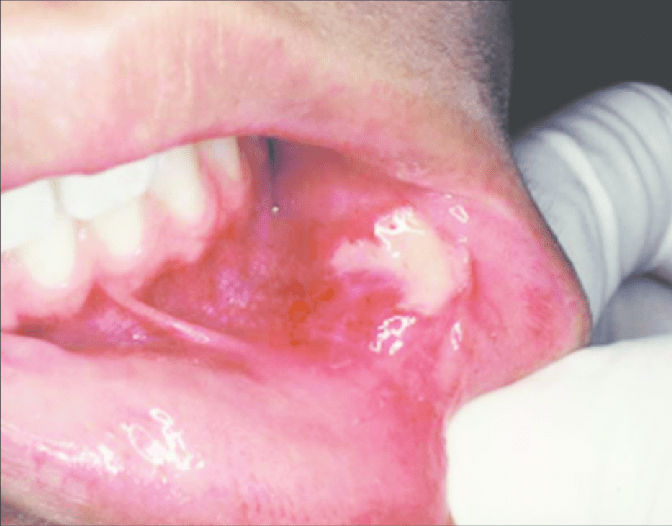
ORAL MANIFESTATIONS
- The most common single site of involvement is the oral mucosa.
- Recurring oral ulcers appear in over 90% of patients; these lesions cannot be distinguished from RAS .
- Some patients experience mild recurring oral lesions; others have the deep large scarring lesions characteristic of major RAS.
- These lesions may appear anywhere on the oral or pharyngeal mucosa.
Histologic Features
The microscopic findings are not diagnostic. They consist of parakeratosis, acanthosis, and polymorphonuclear leukocyte infiltration of epithelium, sometimes with mi- croabscess formation similar to psoriasis. The connective tissue shows a lymphocyte and plasma cell infiltrate.
Laboratory Findings
The patients usually have a mild leukocytosis, an elevated erythrocyte sedimentation rate, and pyuria.
DIFFERENTIAL DIAGNOSIS
- Sweet Syndrome : oral ulcers, conjunctivitis, episcleritis, Inflamed tender skin papules or nodules.
- Erythema Multiforme: erosions, target(iris) lesions.
- Pemphigoid: bullae, erosions.
- Pemphigus : erosions, flaccid skin bullae.
- Reiter syndrome: ulcers, conjunctivitis,
- Herpes simplex virus
- Lupus erythematosus
TREATMENT
The management of Behçet’s syndrome depends on the severity and the sites of involvement.
- Azathioprine combined with prednisone has been shown to reduce ocular disease as well as oral and genital involvement.
- Pentoxifylline, which has fewer side effects than do immunosuppressive drugs or systemic steroids, has also been reperted to be effective in decreasing disease activity, particularly of oral and genital lesions.
- Dapsone, colchicines and thalidomide have also been reported to be effective to treat mucosal lesions of Behcet’s disease.
REFERENCE- BURKET TEXTBOOK OF ORAL MEDICINE AND SHAFER’S TEXTBOOK OF ORAL PATHOLOGY {8TH EDITION}