Dr. Mehnaz Memon🖊
Dentowesome 2020
References: Davidson’s Principles and Practice of Medicine Textbook





Dr. Mehnaz Memon🖊
Dentowesome 2020
References: Davidson’s Principles and Practice of Medicine Textbook

(A)
(B)
5. Regular exercise: Jogging & swimming – ⬇️ Arterial pressure
• Objectives
🔅 To reduce the incidence of adverse cardiovascular events viz coronary heart disease, stroke & heart failure
• Benefits:
🔅Diuretics or β blockers have shown to reduce the risk of
🔅Most of the excess Morbidity & Mortality associated with HT is attributable to CAD. Total CVR = CAD risk x 4/3
🔅 Hypertension in old age:
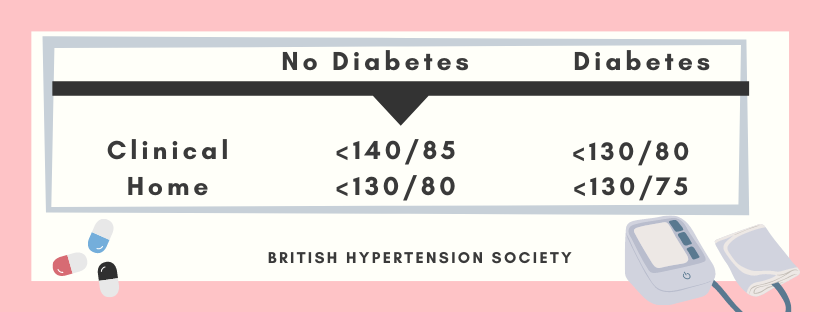
Target BP during AHT



A. ACE Inhibitors:
👉🏻Patients with renal artery stenosis/impaired Renal function (given with utmost care)
⬇️
Reduction of filteration pressure in the glomeruli
⬇️
Renal failure
👉🏻These agents also reduce the progression of Nephropathy in type II diabetes
👉🏻Level of electrolytes & creatinine should be checked before & after 1-2 weeks.
B. ARB’s
👉🏻Have lesser side effects of cough & angioedema than ACE inhibitors
C. Beta-blockers:
👉🏻These drugs are not used now as first line AHT; except in patient with Angina
👉🏻Labetalol & Carvedilol: Have better effect when combined. Labetalol is used as infusion in malignant phase HT.

D. CCB’s
👉🏻The dihydropyridines are effective, well-tolerated particularly in older people
👉🏻Rate–limiting CCB’s: HT with angina. Bradycardia may occur
E. Thiazides & other Diuretics:
👉🏻The loop diuretics have few A/D over thiazides unless there’s renal impairment.

Chart showing Mode of Action & Side effects of AHT’s☝🏻

The influence of comorbidity on the choice of antihypertensive drug therapy

Management of hypertension: British hypertension society guidelines
Criteria:
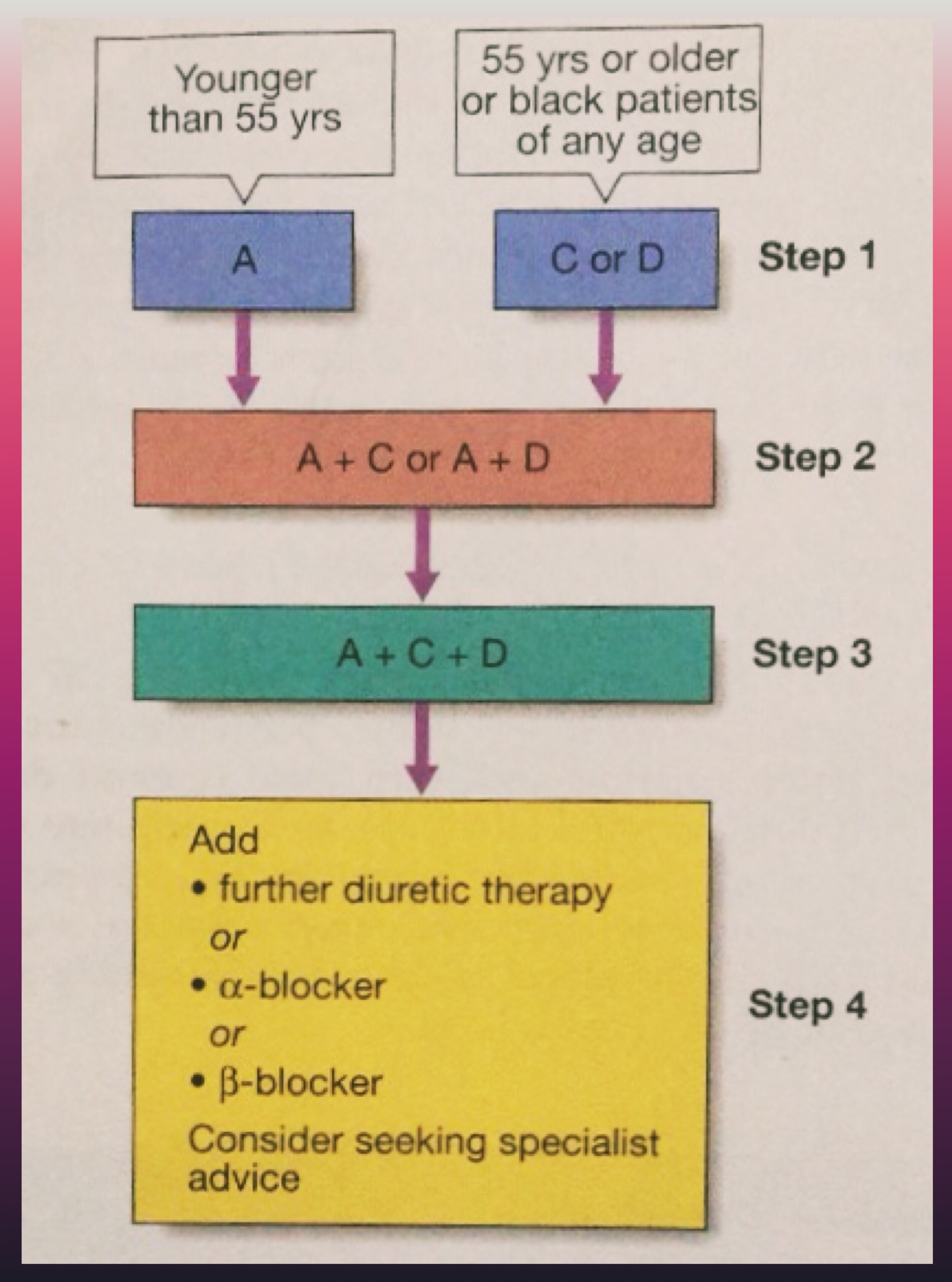
A = ACE inhibitor (consider AT-II receptor antagonist if ACE-intolerant); C = Calcium channel blocker; D = thiazide-type diuretic)
🔅 In accelerated phase HT, lowering BP too quickly may compromise tissue perfusion & can cause –
🔅150/90 mm Hg within 48 hours is ideal along with cardiac failure/hypertensive encephalopathy
🔅Avoid parenteral therapy
🔅Causes of treatment failure include:
📌Aspirin – Antiplatelet
📌Statins – Reduced risk by treating hyperlipidaemia
Dr. Mehnaz Memon🖊
References: Davidson’s Principles and Practice of Medicine Textbook

Hypertension
Definition
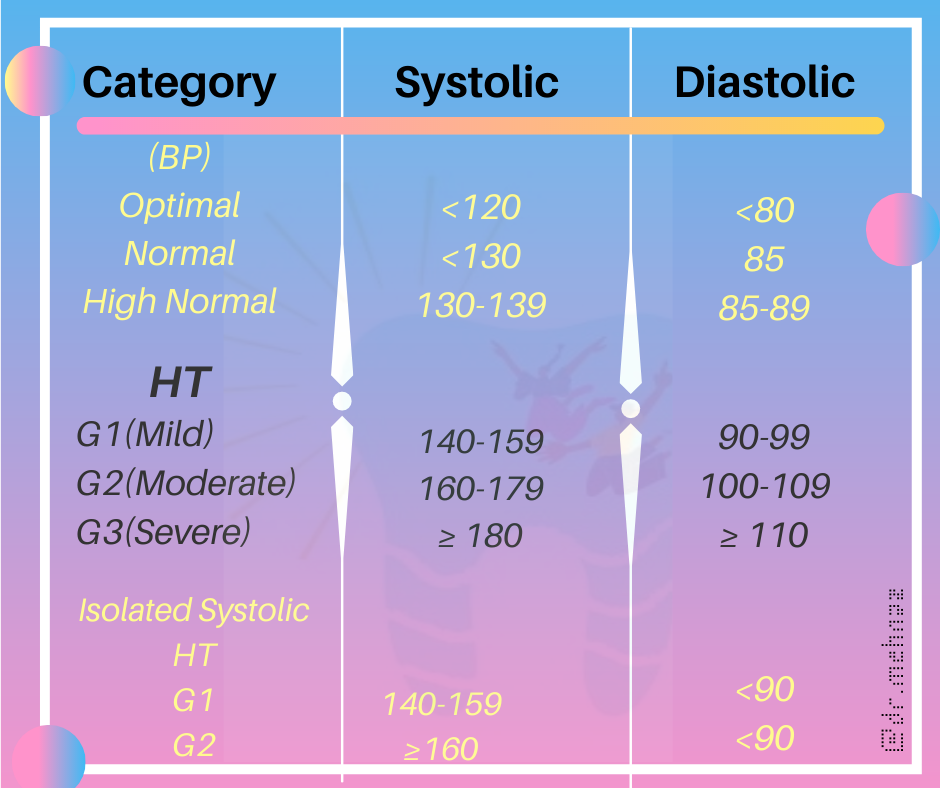
British Hypertension Society
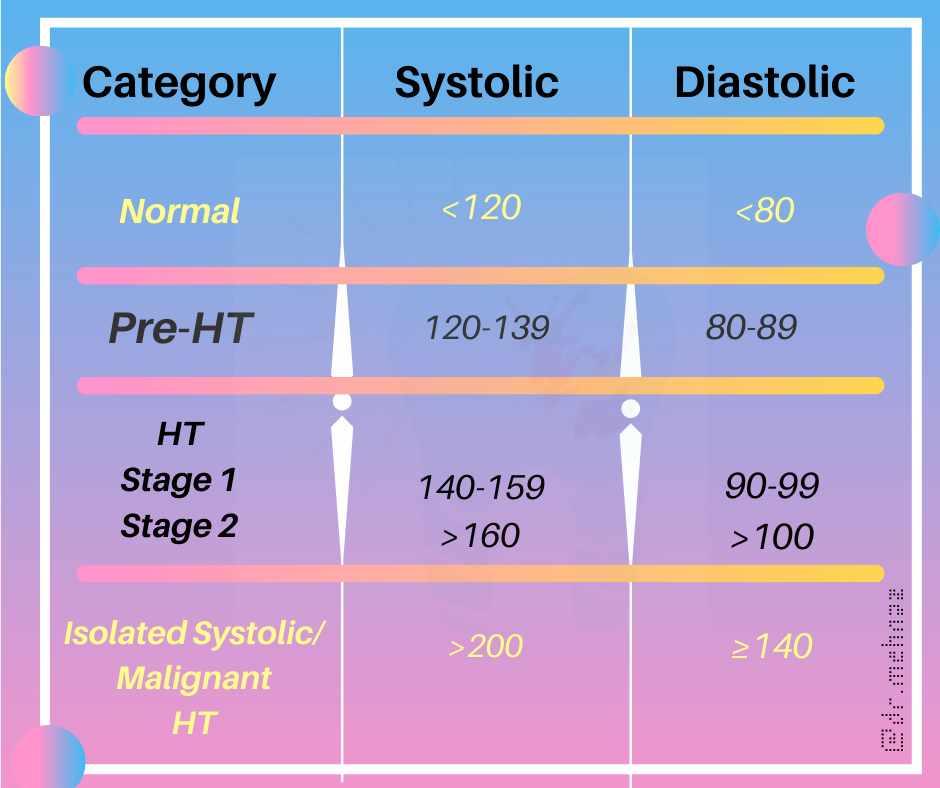
Clinical Classification
References:
Davidson’s Principles and Practice of Medicine Textbook






References:
Davidson’s Principles and Practice of Medicine Textbook


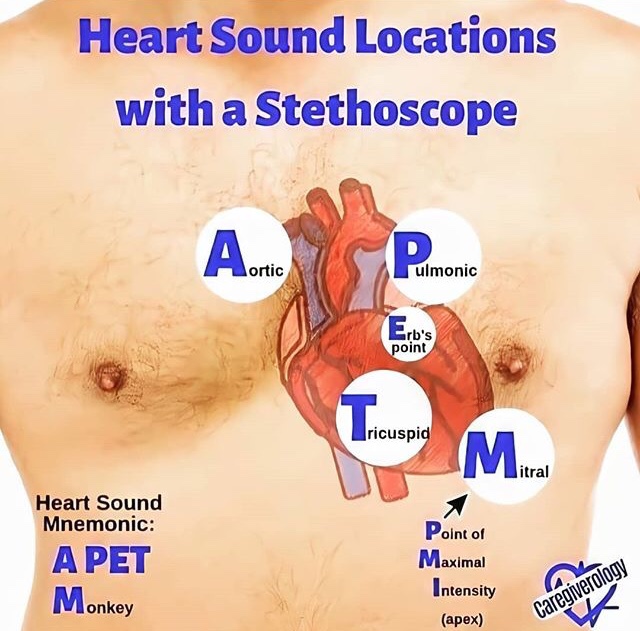
Step 1 – Choose the right equipment:
What you will need:
1. A quality stethoscope
2. An appropriately sized blood pressure cuff
3. A blood pressure measurement instrument such as an aneroid or mercury column sphygmomanometer or an automated device with a manual inflate mode.
Step 2 – Prepare the patient:Make sure the patient is relaxed by allowing 5 minutes to relax before the first reading. The patient should sit upright with their upper arm positioned so it is level with their heart and feet flat on the floor. Remove excess clothing that might interfere with the BP cuff or constrict blood flow in the arm. Be sure you and the patient refrain from talking during the reading.
Step 3 – Choose the proper BP cuff size: Most measurement errors occur by not taking the time to choose the proper cuff size. Wrap the cuff around the patient’s arm and use the INDEX line to determine if the patient’s arm circumference falls within the RANGE area. Otherwise, choose the appropriate smaller or larger cuff.
Step 4 – Place the BP cuff on the patient’s arm: Palpate/locate the brachial artery and position the BP cuff so that the ARTERY marker points to the brachial artery. Wrap the BP cuff snugly around the arm.
Step 5 – Position the stethoscope: On the same arm that you placed the BP cuff, palpate the arm at the antecubical fossa (crease of the arm) to locate the strongest pulse sounds and place the bell of the stethoscope over the brachial artery at this location.
Step 6 – Inflate the BP cuff:Begin pumping the cuff bulb as you listen to the pulse sounds. When the BP cuff has inflated enough to stop blood flow you should hear no sounds through the stethoscope. The gauge should read 30 to 40 mmHg above the person’s normal BP reading. If this value is unknown you can inflate the cuff to 160 – 180 mmHg. (If pulse sounds are heard right away, inflate to a higher pressure.)
Step 7 – Slowly Deflate the BP cuff: Begin deflation. The AHA recommends that the pressure should fall at 2 – 3 mmHg per second, anything faster may likely result in an inaccurate measurement.
Step 8 – Listen for the Systolic Reading: The first occurence of rhythmic sounds heard as blood begins to flow through the artery is the patient’s systolic pressure. This may resemble a tapping noise at first.
Step 9 – Listen for the Diastolic Reading: Continue to listen as the BP cuff pressure drops and the sounds fade. Note the gauge reading when the rhythmic sounds stop. This will be the diastolic reading.
Step 10 – Double Check for Accuracy: The AHA recommends taking a reading with both arms and averaging the readings. To check the pressure again for accuracy wait about five minutes between readings. Typically, blood pressure is higher in the mornings and lower in the evenings. If the blood pressure reading is a concern or masked or white coat hypertension is suspected, a 24 hour blood pressure study may be required to assess the patient’s overall blood pressure profile.
Further Reading/References:
https://www.suntechmed.com/support/product-training-tutorials/1692-how-to-measure-blood-pressure



References:
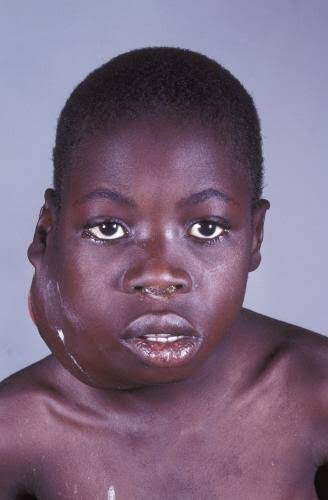
It is also called as ‘African jaw lymphoma’. It is a lymphoreticular cell malignancy. In the African form jaw involvement is 75% and in cases of the American form, abdomen involvement is more common. It is a B-cell neoplasm.
Etiology
• Epstein-Barrvirus(EBV)which also causes nasopharyn- geal carcinoma and infectious mononucleosis is considered to be the etiological factor. There are higher EBV antibody levels in patients of Burkitt’s lymphoma.
Clinical Features
Oral Manifestations
Histology
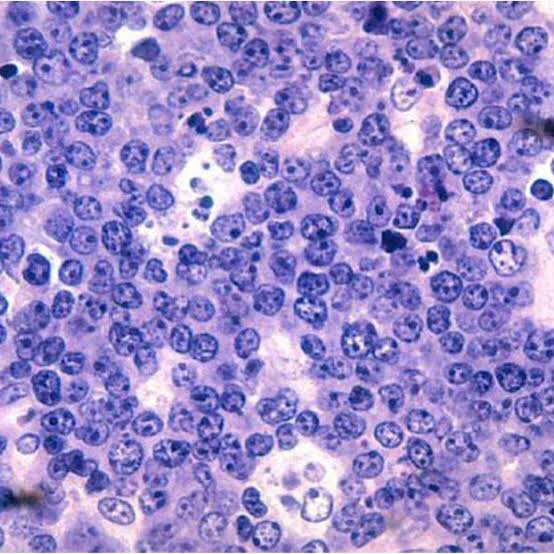
Shows characteristic starry sky appearance.

• Radiological diagnosis—moth eaten appearance is seen with loss of lamina dura around the teeth.
• Laboratorydiagnosis—monotonous sea of un differentiated monomorphic lymphoreticular cells, usually showing abundant mitotic activity. There is also hyperchro- matosis and loss of cohesiveness. Characteristic ‘starry sky’ appearance is seen.
Management
• Cytotoxicdrugs—cytotoxicdrugs like cyclophosphamide 40 mg/kg in single IV administration and repeated about 2 weeks later. Vincristine and methotrexate have been successful in some cases.
• Multiagent chemotherapy—combination of drugs such as cyclophosphamide, vincristine and methotrexate give better results than any single drug. Majority of patients show dramatic response to the therapy. The swelling regresses and the displaced teeth return to their normal position within 1 to 2 weeks.
REFERENCE- SHAFER’S TEXTBOOK OF ORAL PATHOLOGY AND ANIL GHOM TEXTBOOK OF ORAL MEDICINE
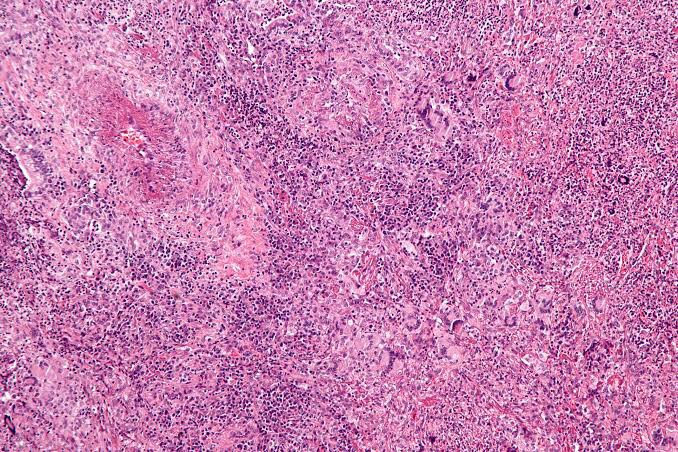
Hodgkin’s Lymphoma
Hodgkin’s disease (HD) is a lymphoid malignancy characterized by the presence of Reed-Sternberg cells of B cell origin. The disease arises usually in single nodal area and successively spreads to contiguous lymph node areas. Extranodal involvement is rare.
Types (Histological)
• Lymphocyte predominant—abundant lymphocytes, few plasma cells, occasional Reed-Sternberg cell, localized involvement of one side of diaphragm and most favorable prognosis.
• Mixed cellularity—lymphocytes, plasma cells, eosino- phils, easily identified Reed-Sternberg cell.
• Nodular sclerosis—sparse lymphocytes, stromal cells, fibrosis and numerous but bizarre Reed-Sternberg cells. It has poor prognosis.
• Lymphocyte depletion—lymphocytes, plasma cells, eosinophils with localized involvement.
ETIOLOGY
CLINICAL FEATURES
Hodgkin’s lymphoma. This high-power photomicrograph shows the characteristic Reed-Sternberg cell (arrow) of Hodgkin ‘s lymphoma, identifiedby its “owl-eye” nucleus.
Diagnosis
MANAGEMENT
Localized disease: The patients with localized disease (IA, IIA) are treated with 3 cycles of chemotherapy (ABVD-doxorubicin, bleomycin, vinblastine and dacarbazine) followed by radiotherapy of involved nodal areas.
Extensive disease: Patients with B symptoms or extensive disease receive complete course (6-8 cycles) of ABVD chemotherapy.
Long-term cure can be achieved in >90% patients with localized disease and in 50-75% patients with extensive disease.
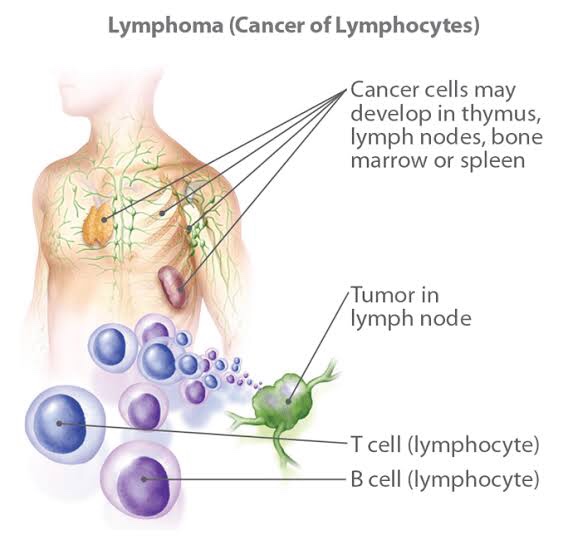
Non-Hodgkin’s Lymphoma
It is also called as ‘lymphosarcoma’. In this group, there is neoplastic proliferation of lymphoid cells, usually affecting the B-lymphocytes. Unlike Hodgkin’s lymphoma, the disease is frequently widespread at the time of diagnosis, often involving not only the lymph nodes but also bone marrow, spleen and other tissue. Early involvement of bone marrow is typical of this lymphoma.
Types (Histological)
The matted, nontender lymph node enlargement in the lateral cervical region represents a common presentation of lymphoma.
Oral manifestations
Radiographic Features
• Appearance—asthediseaseprogressessmallradiolucent foci scattered throughout the area may be seen. Subsequent radiographs of the expanding lesion will show that these small foci have coalesced to form large multilocular moth eaten radiolucency with poorly defined margins.
• Margins—lesion blends imperceptibly with adjacent normal bone, in most of the cases.
• Effect on surrounding structures—lesions may cause marked expansion of bone. Erosion and perforation of cortex may occur.
• Maxillary sinus involvement—if the lesion involves maxillary sinus, possible opacification with breached cortical walls and associated paracentral or intracentral mass.
• Teeth—cortices of unerupted tooth buds and lamina dura of adjacent teeth are lost. Teeth may be resorbed.
Diagnosis
Treatment
The disease stage is determined after clinical evaluation and investigations.
Treatment of low grade lymphoma: It depends on the stage of the disease and clinical status.
REFERENCE- SHAFER’S TEXTBOOK OF ORAL PATHOLOGY, ANIL GHOM TEXTBOOK OF ORAL MEDICINE AND GOGLE SLIDE SHARE
Reiter’s syndrome is associated with urethritis, balanitis, conjunctivitis, and mucocutaneous lesions.
It is a disease of unknown aetiology, although there is evidence of an infec- tious origin.
It is one of the most common complications of non-specific urethritis and it clinically mimicks gonorrhoea, although the urethral discharge is negative for Neisseria.

CLINICAL FEATURES
>Reiter’s syndrome is more prevalent in young adult men, usually between 20 and 30 years of age.
>The male-to-female ratio is 9:1.
>There is a typical tetrad of manifestations: non- gonococcal urethritis, arthritis, conjunctivitis, and mucocutaneous lesions.
>Urethritis may be the first sign. The urethral discharge is usually associated with itching and burning sensation.
>The arthritis is often bilaterally symmetrical and usually polyarticular.
>Conjunctivitis is often so mild as to be overlooked.
>The skin lesions are similar to those seen in keratoderma blennorrhagica and consist of red or yellow keratotic macules or papules which eventually desquamate.
Oral Manifestations
Sites—it is seen on the buccal mucosa, lips and gingiva.
Oral lesions appear as painless, red, slightly elevated areas, some- times granular or even vesicular, with a white circinate border on the buccal mucosa, lips, and gingiva.
The palatal lesions appear as small, bright red purpuric spots, which darken and coalesce, while the lesions on the tongue closely resemble ‘geographic’ tongue.

Laboratory Findings
The patients usually have a mild leukocytosis, an elevated erythrocyte sedimentation rate, and pyuria.

REFERENCE- SHAFER’S TEXTBOOK OF ORAL PATHOLOGY [8TH ED} AND ANIL GHOM TEXTBOOK OF ORAL MEDICINE
Wegener’s granulomatosis is a disease of unknown aetiology, which basically involves the vascular, renal and respiratory systems. It involves the nose, paranasal air sinuses, lower respiratory tract, gut, joints, nervous system, and kidneys. Involvement of the kidney is the common cause of death.
This disease is caused by an abnormal immune reaction secondary to a nonspecific infection or a hypersensitivity reaction to an unknown antigen.

Clinical Features
>Wegener’s granulomatosis may occur at any age, although the majority of cases are in the fourth and fifth decadesof life.
>There is a slight predilection for occurrence in males.
>It is best described as a multisystem disease, which is usually first characterized clinically by the development of rhinitis, sinusitis, and otitis or ocular symptoms.
>The patient soon develops a cough and hemoptysis as well as fever and joint pain.
>Hemorrhagic or vesicular skin lesions are also commonly present.
>Granulomatous lesions of the lungs are found on the chest radiograph, while the glomerulonephritis, which develops ultimately, leads to uraemia and terminal renal failure.
>In nervous system, sensory neuropathy may be an occasional finding.
>Prognosis—the disease is usually fatal, with mean survival time of 5 months. Death occurs due to involvement of kidney.
Oral Manifestations
Involvement of the gingiva has been the most common and characteristic manifestation, and is termed as strawberry gingivitis.Gingival lesions may manifest as ulcerations, friable granular lesions, or simply enlargements of the gingiva.
The inflammatory process starts in the interdental papilla and spreads rapidly to the periodontal structure and leads to bone loss and tooth mobility.
Palate—orallesionstypicallyincludeulcerationofthe palate by extension of nose lesions and destruction of nasal septum. This will lead to perforation of palate.
• Teeth—theremaybelooseningofteethwithinsomecases spontaneous exfoliation. After extraction of teeth patient is usually noticed poor healing.

Laboratory Findings
Laboratory findings include anaemia, leukocytosis, elevated erythrocyte sedimentation rate, and hyperglobulinaemia. Because of kidney involvement, haematuria is common, as well as the finding of albumin, casts, and leukocytes in the urine. Circulating immune complexes have been demonstrated in some patients, but this is not a consistent finding.
Histologic Findings
Wegener’s granulomatosis presents a pattern of mixed inflammation centred around the blood vessels.
The lesions in the upper respiratory tract and lungs consist of giant cell necrotizing granulomatous lesions showing vasculitis.
Oral biopsy specimens show pseudoepitheliomatous hyperplasia and subepithelial abscesses. The gingival and other lesions show a nonspecific granulomatous process with scattered giant cells.
Diagnosis
REFERENCE- SHAFER’S TEXTBOOK OF ORAL PATHOLOGY {8TH ED} AND ANIL GHOM TEXTBOOK OF ORAL MEDICINE