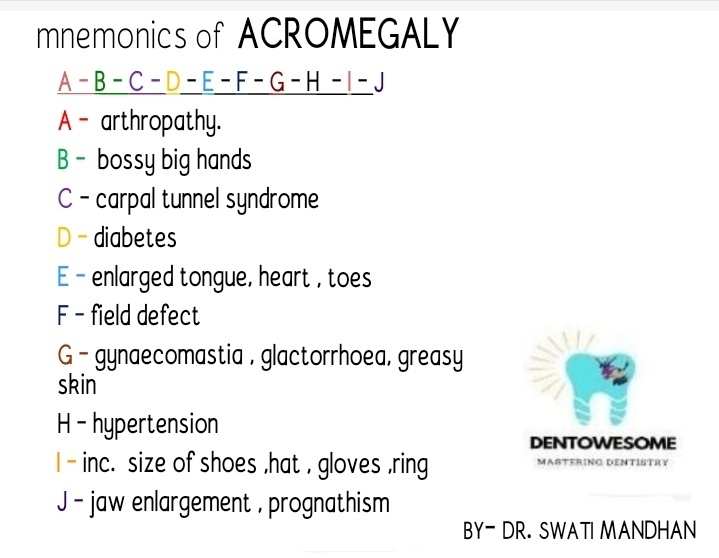

Sign and symptoms of acromegaly [ mnemonics]
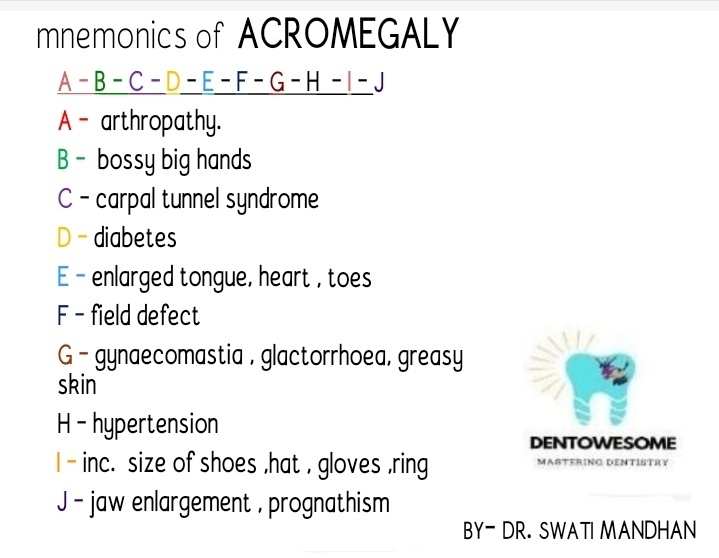

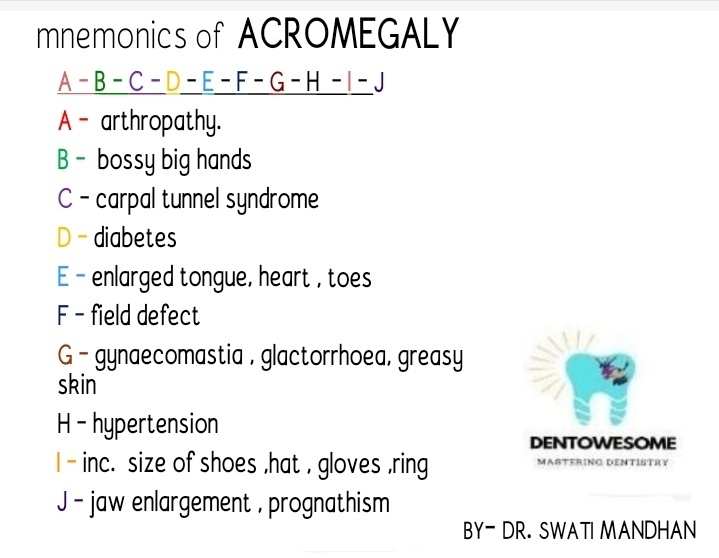



Reference- Davidson’s Principles & Practice Of Medicine
Between Portal and Systemic Veins. Sites are:
1. At the lower end of oesophagus – esophageal tributaries of left gastric vein ( portal) communicate with oesophageal tributaries of hemiazygous veins (systemic).
2. At the lower end of rectum and anal canal – superior rectal vein (portal) communicates with middle and inferior rectal veins (systemic).
3. Anterior abdominal (around umbilicus):
4. At bare area of liver – portal radicles of liver communicates with diaphragmatic veins (systemic)
5. At retroperitoneal site – the splenic and colic veins (portal) communicate with renal veins and other tributaries of IVC by small veins, called veins of Retzius.
6. At the fissure for ligamentum venosum, rarely, persistent ductus venosus establishes direct portocaval anastomosis (in fetal life, left branch of portal vein at the porta hepatitis communicates with IVC via ductus venosus. After birth, ductus venosus is fibrosed to form ligamentum venosum).
It consists of central arteriole from which numerous capillaries radiate, looks kike spider legs. Size varies from pinhead to 1-2 mm (sometimes cm). These are found along the area of SVC, commonly in neck, face, chest, and dorsum of hand and above nipple lines, cause of which is not known. It blanches on pressure, may pulsate if large. Better seen with glass slide or pinhead.
Causes of spider angioma:
1. Physiological:
2. Pathological:
Mechanism of spider angioma:
Differential diagnosis of spider angioma:
These are 2-3 cm lesions that occur on dorsum of foot, leg, back and lower chest. Caused by elevated venous pressure amd are usually found overlying the main tributary of large veins. Do not blanch on pressure and blood flow if from periphery to the center of lesion (opposite to spider angioma).
Redness in thenar and hypothenar eminence and pulp of fingers. Blanches of pressure. With glass slide, flushes synchronously with pulse. Causes of palmar erythema:
1. Physiological:
2. Pathological:
Mechanism of palmar erythema:
Reference: Clinical Medicine – ABM Abdullah

1. Trigeminal Neuralgia
2. Post-herpetic Neuralgia
3. Giant-cell Arteritis
4. Other causes of facial pain
5. Approach to facial pain diagnosis
LINK:⬇️

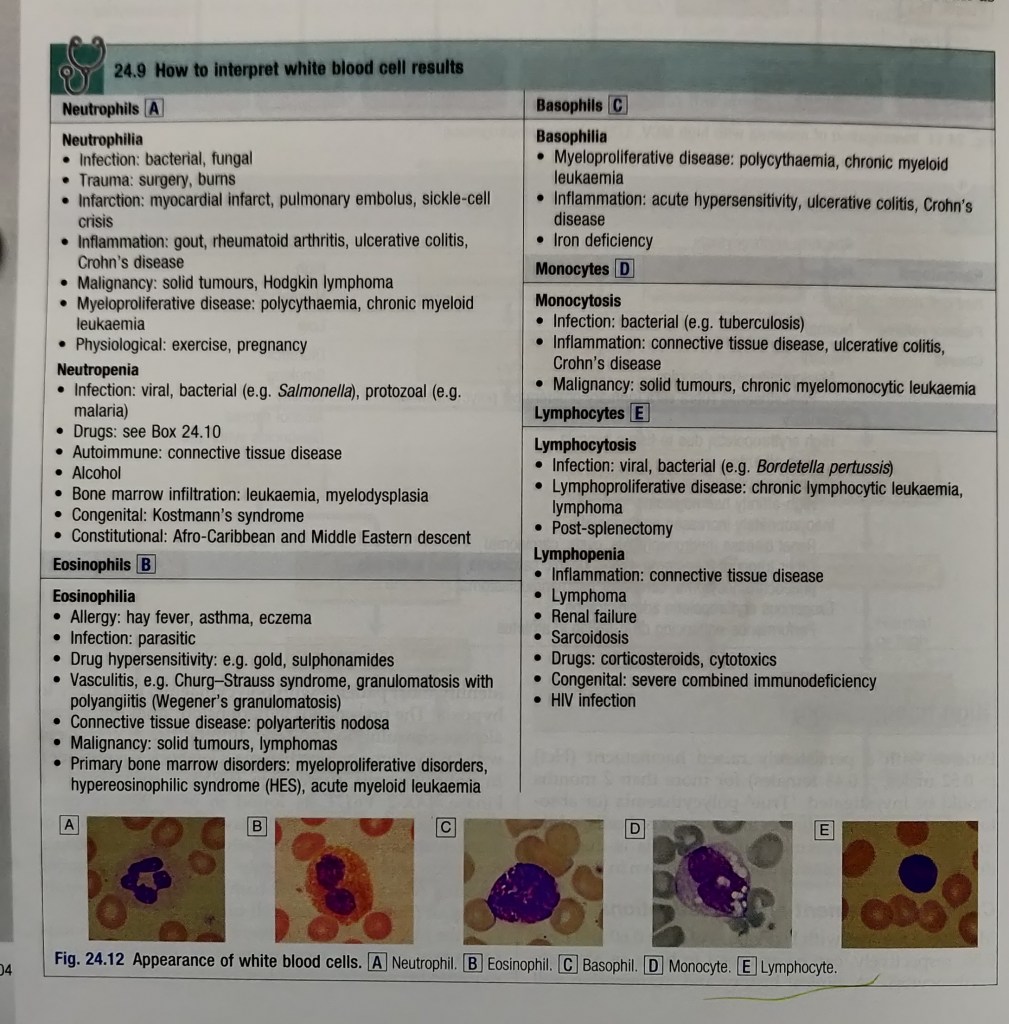
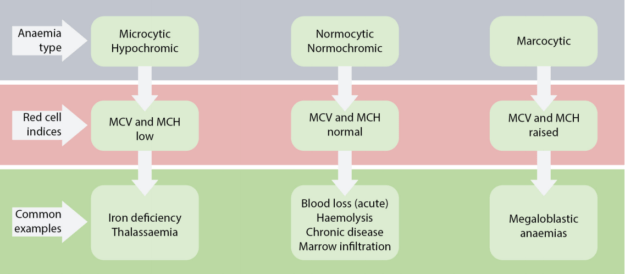
• Also known as: CBC; Hemogram
• Sample Required?
• Test Preparation Needed?
• Why get tested?
• Also known as: Hgb; Hb; H and H (Hemoglobin and Hematocrit)
• Sample Required?
• Test Preparation Needed?
• Why get tested?
• When to get tested?
• Also known as: Thrombocyte count; PLT; Platelet distribution width; PDW; Mean Platelet volume; MPV.
• Sample Required?
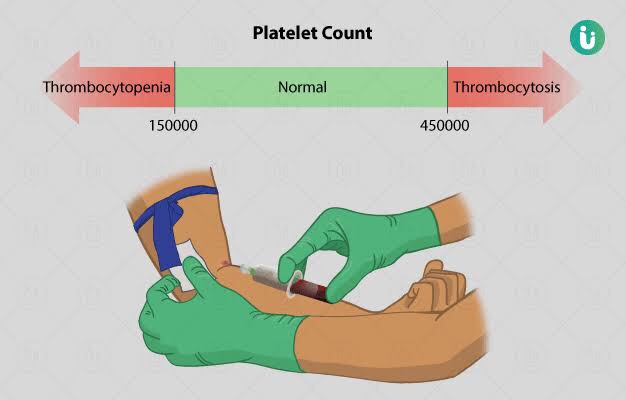
• Test Preparation Needed?
• Why get tested?

• When to get tested?
• What is being tested?

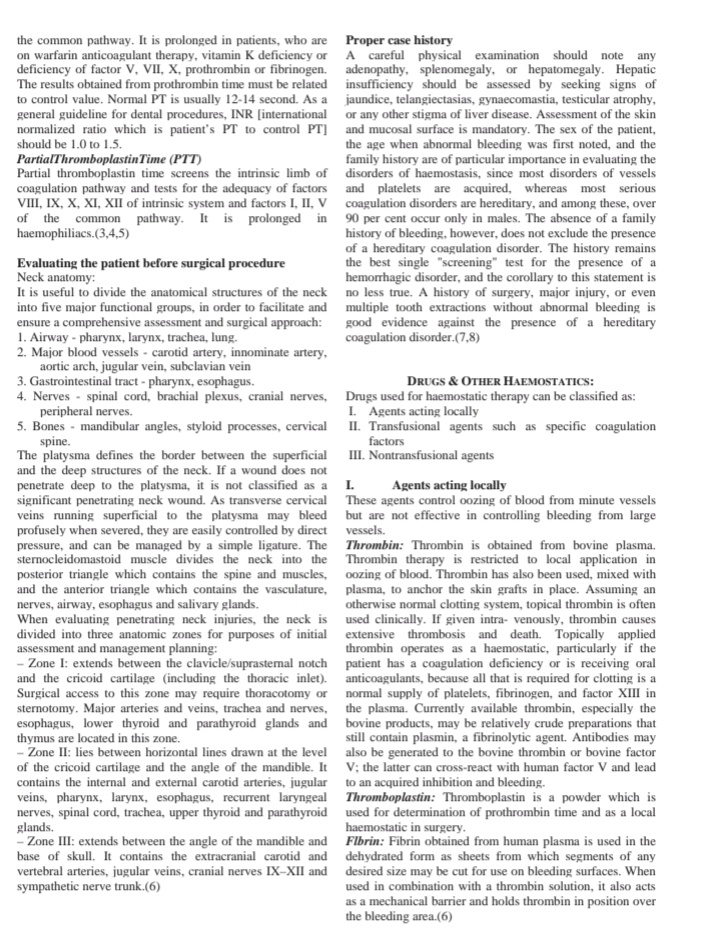
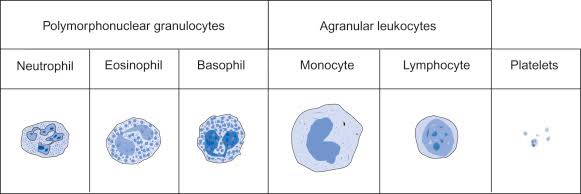
• Also known as: Leukocyte differential count; Peripheral differential; WBC count differential; Diff; blood differential; Differential Blood Count
• Formal name: White blood cell differential
• Why get tested?
• When to get tested?
• What is being tested?

Dentowesome|@drmehnaz🖊
References: Google.com, lecturio.com, Study Notes✍🏻
Muhad Noorman p, Final year, Team Dentowesome
Hyperparathyroidism
Disorder of parathyroid gland characterised by excess secretion of PTH hormones resulting in clinical and biochemical hypercalcemia.
The most common cause of excess hormone production (hyperparathyroidism) is the development of a benign tumor in one of the parathyroid glands. This enlargement of one parathyroid gland is called a parathyroid adenoma which accounts for about 70 percent of all patients with primary hyperparathyroidism. The other causes comprises of parathyroid hyperplasia and PARATHYROID carcinoma (rarely).
Types
1) Primary hyperparathyroidism occurs when there is a disorder of the parathyroid glands themselves.
2) Secondary hyperparathyroidism results when a condition elsewhere in the body affects the parathyroid glands, causing them to produce too much hormone
3) Teritiary hyperparathyroidism causes when long standing secondary hyperparathyroidism become autonomous gland
CLINICAL FEATURES
Commonly found in middle aged women’s.
Hyperparathyroidism may or may not cause symptoms. When symptoms do appear, they are often mild, such as
weakness,
fatigue,
depression,( psychic moans) or
body aches and pains.
In primary hyperparathyroidism, the elevated levels of PTH cause elevated levels of blood calcium (hypercalcemia). Increased calcium and phosphorus excretion in the urine may cause kidney stones.(Nephrocalcinosis and nephrolithiasis).
Diagnosis of hyperparathyroidism relies on blood tests to measure hormone and calcium levels. Elevated Serum Calcium and phosphorus level .
Surgery is the main treatment for hyperparathyroidism. Surgical resection of adenoma and transplantation in hand muscles is most followed protocol .
Reference; Internet, SRB Textbook of surgery

Antibiotics can be divided into 2 classes based on their mechanism of action:-
➡️ Bactericidal antibiotics kill bacteria by inhibiting cell wall synthesis. Example:
➡️ Bacteriostatic antibiotics limit the growth of bacteria by interfering with bacterial protein production, DNA replication or other aspects of bacterial cellular metabolism.
They must work together with immune system to remove the micro-organisms from the body. Example:
Note that while it is rational to favor bactericidal agents over bacteriostatic agents, neither has ever been shown to be superior (probably because true recovery from infection cannot occur until the body is able to mount an appropriate immune response, thus “buying time” may be just as good as active killing)
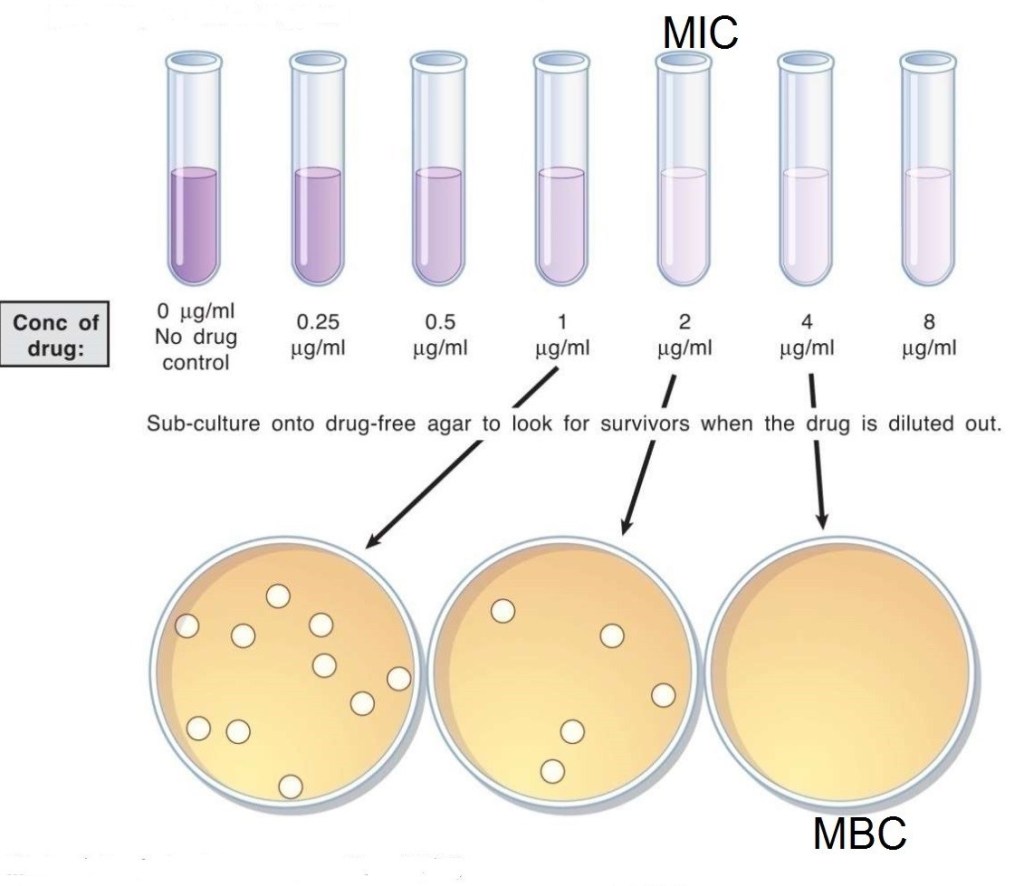
➡️ The MBC is the minimum concentration of drug which can kill the micro-organisms.
➡️ The MIC is the minimum concentration of drug which can inhibit the growth of micro-organisms.
Council for Appropriate and Rational Antibiotic Therapy (CARAT) criteria for accurate use of antibiotic therapy
● Evidence-based results ●Therapeutic benefits
● Safety
● Cost-effectiveness
● Optimal drug dose and duration —Shorter-course, more aggressive therapy
(i) Evidence-based results:
In choosing an antibiotic, clinicians should consider the clinical evidence demonstrating that the drug is clinically and microbiologically appropriate, the efficacy of that drug in well-designed clinical trials, and the antibiotic resistance patterns of the local region. Clinicians should then use their professional judgment to choose the optimal antibiotic.
(ii) Therapeutic benefits:
If possible, the clinician should identify the causative pathogen and use surveillance data on regional antibiotic resistance patterns in selecting the optimal therapeutic agent.
(iii) Safety:
In treating patients with a particular drug, safety must be weighed against efficacy. Clinically applicable treatment strategies should be chosen to maximize efficacy while minimizing side effects.
(iv) Optimal drug for optimal duration:
Optimal drug selection requires finding the antimicrobial class and the specific member of that class that is best suited to treat a particular infection. Because empiric therapy is necessary in most cases, multiple factors have to be considered. Among these are whether the etiologic agent is likely to be gram-positive or gram-negative, whether a narrow or broad-spectrum agent should be chosen, the resistance patterns of the likely pathogen to this drug, both nationally and regionally, and the individual patient’s medical history, including recent antibiotic exposure.
Optimal duration means prescribing the selected drug for the shortest amount of time required for clinical and micro- biologic efficacy. There are many reasons for reducing an- timicrobial therapy to the shortest appropriate duration. They include the potential for reduced occurrence of adverse effects, increased patient adherence, decreased promotion of resistance, and decreased costs.
(v) Cost-effectiveness:
Choosing inappropriate therapy is associated with increased costs, including the cost of the antibiotic and increases in overall costs of medical care because of treatment failures and adverse events.
Dentowesome | @drmehnaz🖊
References:
MUHAD NOORMAN P, final year, Team dentowesome


Reference: DAVIDSONS INTERNAL MEDICINE 20TH ED