A 58-year-old man gave a history of stabbing pain affecting his left temple. Each burst of pain lasts for about 4 minutes and he can experience three of these each waking hour. He is concerned that he may have developed an infection in his left eye, which looks red.
On first reading, this case has many of the features of trigeminal neuralgia. The 4-minute duration of the pain is possibly longer than one might normally expect for TN and the ophthalmic is the least commonly affected division of the trigeminal nerve. The presence of conjunctival infection shifts the balance in favour of short-lasting unilateral neuralgiform headache attacks with conjunctival injection and tearing but an overlap is recognised between the two conditions. MRI indicated.
RESEARCH ARTICLES
Short-lasting unilateral neuralgiform headache attacks (SUNHA) is a rare form of primary headache that falls under the category of trigeminal autonomic cephalalgias (TACs) (Weng et al., 2017). SUNHA is further divided into two subtypes: short-lasting unilateral neuralgiform headache attacks with conjunctival injection and tearing (SUNCT) and short-lasting unilateral neuralgiform headache attacks with cranial autonomic symptoms (SUNA) (Levy & Matharu, 2018). These headache disorders are characterized by severe, short-lasting headaches that occur unilaterally and are accompanied by ipsilateral cranial autonomic symptoms (Goadsby et al., 2007).
SUNCT is characterized by frequent attacks of unilateral, orbital, supraorbital, or temporal stabbing or pulsating pain that lasts for 5 to 240 seconds (Leone et al., 2005). These attacks are often accompanied by conjunctival injection, tearing, and blocked or runny nostril, all on the same side as the pain (Leone et al., 2005). However, it is important to note that not all patients with SUNCT manifest both conjunctival injection and tearing (Weng et al., 2017).
SUNA, on the other hand, is characterized by similar short-lasting unilateral headaches, but with additional cranial autonomic symptoms such as ptosis, miosis, eyelid edema, or nasal congestion (Weng et al., 2017). Like SUNCT, SUNA attacks are also frequent and can last from seconds to minutes (Weng et al., 2017).
The exact cause of SUNHA is not fully understood, but there is evidence suggesting hypothalamic involvement in these conditions (Cohen, 2007). Functional imaging studies have shown activation of the posterior hypothalamus in patients with TACs, including SUNHA (Cohen, 2007). Additionally, deep brain stimulation of the hypothalamus has been used as a treatment option for these headache disorders (Cohen, 2007).
The diagnosis of SUNHA is based on clinical presentation and the exclusion of other possible causes of headache (Goadsby et al., 2007). The International Classification of Headache Disorders (ICHD) criteria are commonly used for diagnosis (Qaiser et al., 2020). However, diagnosing SUNHA in pediatric patients can be challenging due to limited data and the overlap of symptoms with other headache disorders (Ghosh et al., 2021).
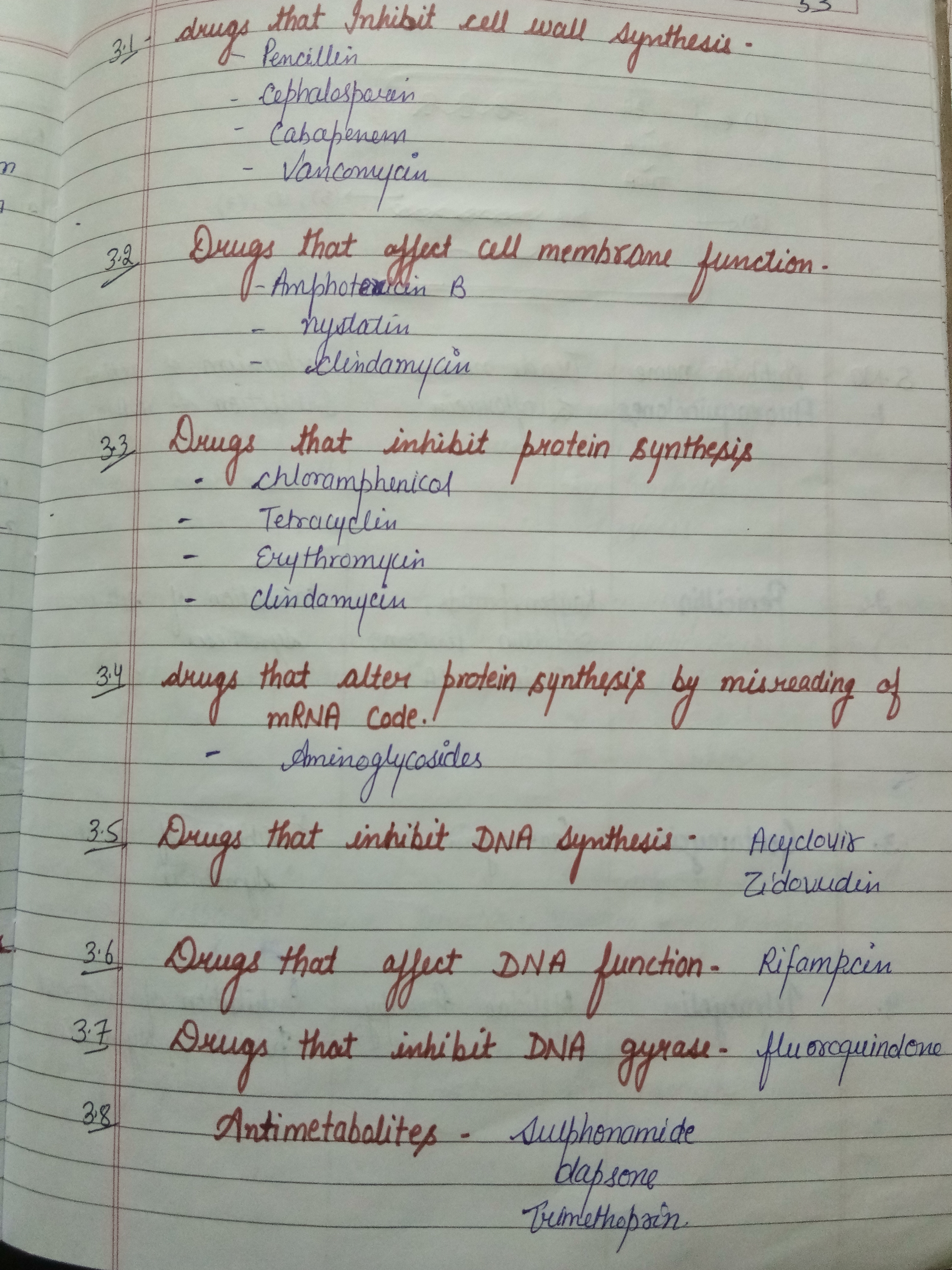
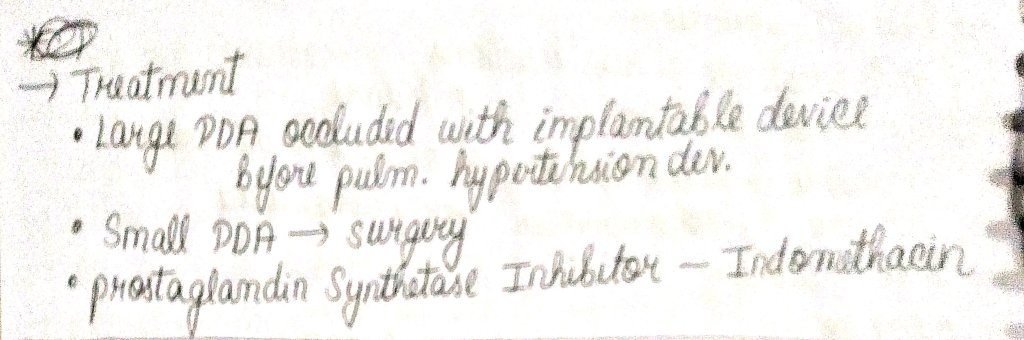
reatment options for SUNHA include both pharmacotherapy and procedural interventions (Pomeroy & Nahas, 2015). Pharmacological preventive treatments have been tried, but there is no specific medication that is universally effective for all patients (Levy & Matharu, 2018). Some commonly used medications include indomethacin, lamotrigine, topiramate, and gabapentin (Wei & Jensen, 2018). In cases where pharmacotherapy is ineffective, procedural interventions such as occipital nerve stimulation or deep brain stimulation may be considered (Miller et al., 2017).
In conclusion, short-lasting unilateral neuralgiform headache attacks (SUNHA) is a rare form of primary headache that falls under the category of trigeminal autonomic cephalalgias (TACs). It is characterized by severe, short-lasting headaches that occur unilaterally and are accompanied by ipsilateral cranial autonomic symptoms. The exact cause of SUNHA is not fully understood, but there is evidence suggesting hypothalamic involvement. Diagnosis is based on clinical presentation and the exclusion of other possible causes of headache. Treatment options include pharmacotherapy and procedural interventions, but there is no universally effective medication for all patients. Further research is needed to better understand the pathophysiology and develop more effective treatments for SUNHA.
References
Cohen, A. (2007). Short-lasting Unilateral Neuralgiform Headache Attacks With Conjunctival Injection and Tearing. Cephalalgia, 7(27), 824-832. https://doi.org/10.1111/j.1468-2982.2007.01352.x Ghosh, A., Silva, E., Burish, M. (2021). Pediatric-onset Trigeminal Autonomic Cephalalgias: a Systematic Review And Meta-analysis. Cephalalgia, 13(41), 1382-1395. https://doi.org/10.1177/03331024211027560 Goadsby, P., Cohen, A., Matharu, M. (2007). Trigeminal Autonomic Cephalalgias: Diagnosis and Treatment. Curr Neurol Neurosci Rep, 2(7), 117-125. https://doi.org/10.1007/s11910-007-0006-6 Leone, M., Franzini, A., D’Andrea, G., Broggi, G., Casucci, G., Bussone, G. (2005). Deep Brain Stimulation To Relieve Drug-resistant Sunct. Ann Neurol., 6(57), 924-927. https://doi.org/10.1002/ana.20507 Levy, A., Matharu, M. (2018). Short-lasting Unilateral Neuralgiform Headache Attacks. Ann Indian Acad Neurol, 5(21), 31. https://doi.org/10.4103/aian.aian_356_17 Miller, S., Watkins, L., Matharu, M. (2017). Long-term Follow Up Of Intractable Chronic Short Lasting Unilateral Neuralgiform Headache Disorders Treated With Occipital Nerve Stimulation. Cephalalgia, 5(38), 933-942. https://doi.org/10.1177/0333102417721716 Pomeroy, J., Nahas, S. (2015). Sunct/suna: a Review. Curr Pain Headache Rep, 8(19). https://doi.org/10.1007/s11916-015-0511-2 Qaiser, S., Hershey, A., Kacperski, J. (2020). Sunct/suna In Children and Adolescents: Application Of Ichd-3 Criteria And Treatment Response: Case Series Of 13 Sunct/suna Pediatric Cases. Cephalalgia, 1(41), 112-116. https://doi.org/10.1177/0333102420954525 Wei, D., Jensen, R. (2018). Therapeutic Approaches For the Management Of Trigeminal Autonomic Cephalalgias. Neurotherapeutics, 2(15), 346-360. https://doi.org/10.1007/s13311-018-0618-3 Weng, H., Cohen, A., Schankin, C., Goadsby, P. (2017). Phenotypic and Treatment Outcome Data On Sunct And Suna, Including A Randomised Placebo-controlled Trial. Cephalalgia, 9(38), 1554-1563. https://doi.org/10.1177/0333102417739304