

Sources: Sturdevants 7th edition


Sources: Sturdevants 7th edition
Several modifications have been proposed for in class II cavity design for amalgam restorations . These modifications are changes from the classic preparation design . They are indicated for those situations which are not ideal. Modifications are based on following factors:
MODIFICATIONS :
2. SLOT PREPARATION : It is similar to class V amalgam cavity preparation except that it is done on the proximal surface of the tooth. It is indicated in proximal root surface caries with gingival recession. The design is similar to that of the slot preparation except it is approached from the facial aspect without disturbing the contact area.
3. CONSERVATIVE DESIGNS : It is recommended in all posterior teeth where caries incidence is very low and all occlusal pits and fissures are not involved. The conservative design preserves all the remaining sound tooth structures such as transverse ridge or oblique ridge and thereby protects the cuspal strength .
4. MODIFICATIONS TO PRESERVE ESTHETICS : To preserve the esthetics in the critical area during a mesio-occlusal cavity preparation , the facial wall of the mesial box should be prepared straight , i.e parallel to the long axis of the tooth rather than gingivally divergent . Another modification is to avoid breaking the facial contact whenever caries is limited only to the mesio-lingual embrassure.
5. MODIFICATIONS OF ROTATED TEETH : Depending on the degree of rotation , the proximal box is displaced facially or lingually.
6. ADJOINING RESTORATIONS : The intersecting margins of the two restorations -should be at right angles . Care should be taken so as to prepare the outline of the new cavity without weakening the amalgam margin of the existing restoration .
7. MODIFICATIONS FOR ABUTMENT TOOTH: The facial and lingual walls of the proximal box must be extended more so that the entire rest seat can be prepared in the amalgam without encroaching on the occlusal margins.
The pulpal floor is deepend an extra 0.5 mm apical to the region of the rest seat so as to provide an adequate thickness of amalgam.
8. CUSP CAPPING : It is indicated where there are extensive caries underneath the cusps and facio-lingual extensions of the occlusal preparation is more than 2/3rd the distance between the facial and lingual cusp tips. For cusp capping 1.5 to 2 mm of cusp reduction is necessary . The reduced cusps must meet the adjacent unreduced cusp at 90 degree cavosurface angle to provide both adequate edge strength of amalgam.
References: STURDEVANTS 7TH EDITION
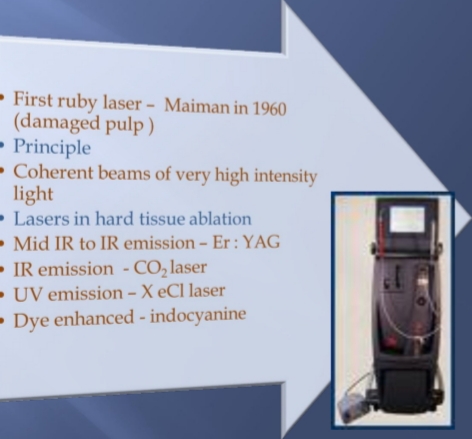
LASER: Light Amplification by Stimulated Emission of Radiation .Laser dentistry is easier, more precise ,less traumatic for patients . Lasers provide a state-of-the-art approach for modern dentistry.
DISCOVERY : It was discovered by Shallow and Towns on 1958. First working laser was built by Maiman of Hughes research laboratory in 1960.
COMPONENTS OF LASER :
BASIC PRINCIPLES OF LASERS
LASER TISSUE INTERACTION :
TYPES OF LASERS :
1.BASED ON WAVELENGTH :
2. BASED ON TARGET TISSUE
LASER APPLICATION IN CONSERVATIVE DENTISTRY :
REFERENCES: STURDEVANTS 7TH EDITION
Written by – Dr. Urusa I Inamdar
A tooth that is difficult to anesthetize is known as a ‘hot tooth ‘. This is most commonly encountered in a mandibular first molar tooth wherein after the anesthetic block , the patient may describe profound numbness of the ipsilateral lip and tongue but still may experience acute pain during the access opening procedure.
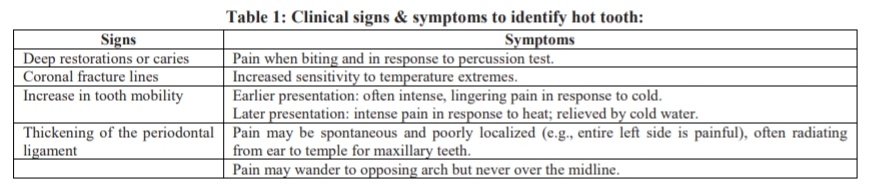
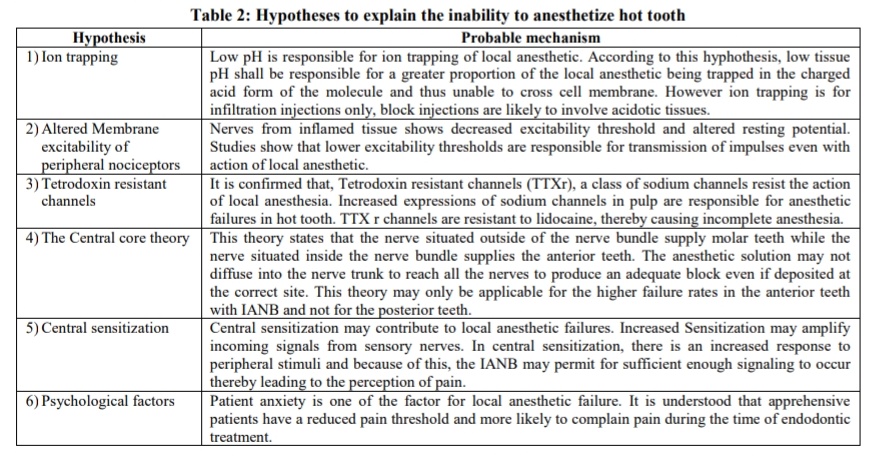
There is a special class of sodium channels on C – fibers, known as tetrodotoxin-resistant (TTXr) sodium channels. The expression shifts from TTX- sensitive to TTXr during neuroinflammatory reactions and the TTXr sodium channels play a role in sensitizing C-fibers and creating inflammatory hyperalgesia. One of the clinically significant characteristics of these sodium channels is that they are relatively resistant to lidocaine. These channels are five times more resistant to anesthetic than TTX- sensitive channels. Hot tooth may be explained by the fact that the TTXr sodium channels have not been adequately blocked by the anesthetic.
Bupivacaine has been found to be more potent than lidocaine in blocking TTXr channels and may be the anesthetic of choice when treating ‘hot tooth.’ Supplemental intraligamentary or intraosseous injections are most helpful to ensure profound local anaesthesia.
References:

Source: Internet
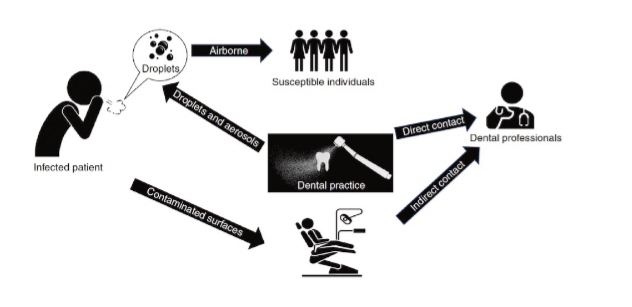
Amidst the pandemic state with the high transmissibility of the disease through air & droplets and considering that routine dental procedures usually generate aerosols; alterations to dental treatment is of prime concern to maintain a healthy environment for patient & dental team.Here is where the approach of performing minimally invasive dental treatment becomes crucial.
What is minimal intervention dentistry?
Minimal intervention dentistry( MID) is a conservative philosophy of professional care concerned with first occurrence,early detection & earliest possible cure of caries at a micro level ; followed by minimally invasive and patient friendly treatment to repair irreversible damage caused by dental caries.
Goals & Principles:

.Early diagnosis of dental caries
.Assessment of individual caries risk
.Disease control by remineralisation of incipient carious lesions.
.Repair rather than replacement of defective restorations
.Minimal invasive treatment
.Periodic follow up.
Caries diagnosis:
Includes early diagnosis & caries risk assessment


Procedures:

Non invasive procedures: Biological approach


Minimal invasive treatments:
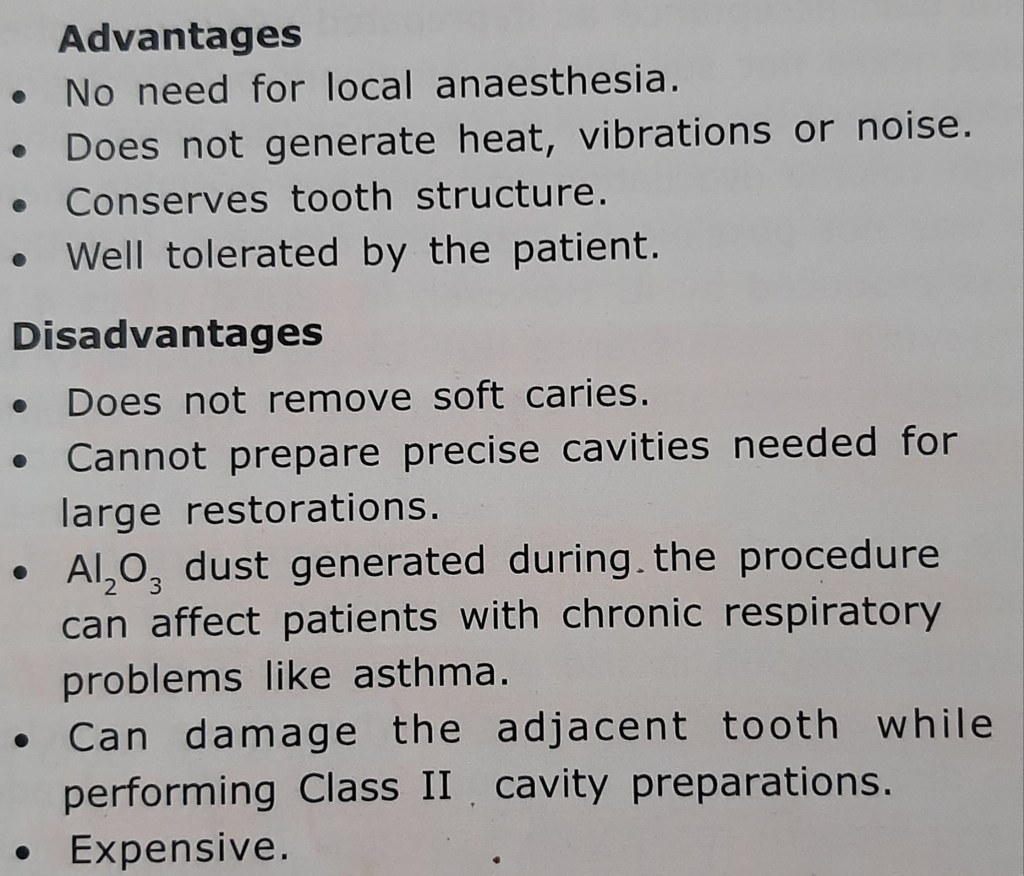
1)Air abrasion
Indications-
.for abrading the surface of old composites prior to new restoration ; minimal class I & class II preparations for composites ; for abrading ceramic or cast restorations for bonding ; for widening pits & fissures for sealants.

2) Sono Abrasion
Indications-
.opening pits & fissures for sealant restorations ; minimal preparation of incipient class II cavities

3) Chemicomechanical Caries Removal (CMC)

Carisolv – 2 syringe system ,one containing NaOCl & other with 3 amino acids (glutamic acid,leucine ,lysine); carboxymethylcellulose gel;NaCl,NaOH;Erythrosine.The contents are mixed together to form a pink gel which is applied onto carious dentin and left in place for 30 seconds to allow it to soften & degrade the infected dentin.
Advantages – relatively painless, removes only carious dentin, no vibrations,better substrate for adhesive bonding
Disadvantages- expensive, time consuming
4)Enzymes
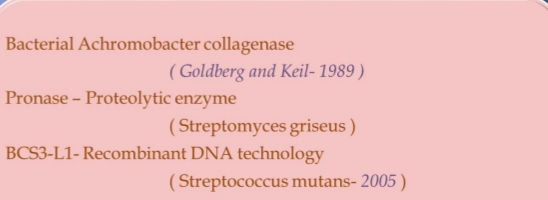
5)Laser
2 commonly developed lasers-
.Er:Cr:YSGG(2780 nm)- Erbium,Chromium,Yttrium,Scandium,Gallium,Garnet laser – works by agonizing water droplets as they travel towards the target tissue.
.Er:YAG(2940nm)-Erbium,Yttrium,Scadium,Aluminum,Garnet laser – uses pulses of light energy to micro vaporize water within the target tissues.

6)Ozone

Caries treatment with ozone – based on Niche environment theory .Ozone kit consists of portable apparatus & disposable silicon cups. Follow up 3-6 months.
Disadvantages – can cause porosities or abrade tooth surface ,in case of heavy exposure.
Other techniques (in brief):
7)Atraumatic restorative treatment (ART)

8)Rotary instruments

Cavity designs for minimal tooth preparation:
According to the new classification based on site,size & severity of lesion,following are the designs –




Restorative materials used in minimal invasive dentistry :

Conclusion:
Minimal intervention techniques cause less tooth destruction than conventional techniques,thus increasing the long term survival of teeth ,also cause less discomfort to the patient and ensure healing of the disease not only the symptoms. With a reduction in chair side time and simplified techniques there is lesser chances of exposure of the dentist to aerosol contamination,thus maintaining which is the need of the hour.
DENTIN HYPERSENSITIVITY :It is characterized by short , sharp pain arising from exposed dentin in response to stimuli typically thermal , chemical, osmotic, evaporative, tactile and which cannot be ascribed to any other form of dental defect or pathology.
ETIOLOGY :
ENAMEL LOSS :
CEMENTAL LOSS:
DEVELOPMENT OF DENTIN HYPERSENSITIVITY
There are two phases in the devlopment of dentin hypersensitivity .
Several theories have been put forward to explain the dentin hypersensitivity.
CLINICAL FEATURES:
DIAGNOSIS :
CASE HISTORY :
CLINICAL EXAMINATION :
PREVENTION :
MANAGEMENT :
DESENSITIZATION BY OCCLUDING DENTINAL TUBULES :
DESENSITIZATION BY BLOCKING PULPAL SENSORY NERVES
REFERENCE: STURDEVANTS 7TH EDITION
Written by- Dr. Urusa I Inamdar

Reference:
Grossman’s Endodontic Practice (13th edition)
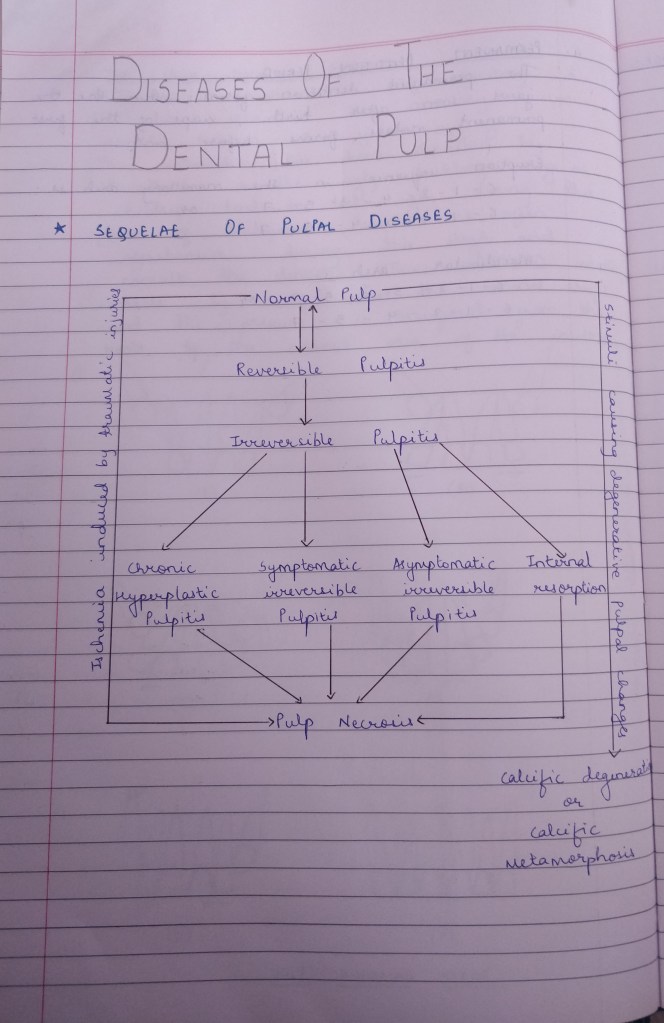
One of the basic goals of conservative dentistry is to preserve the health of the pulp as it is subjected to many insults such as caries, trauma, operative procedures, restorative materials.
Pulpal irritants can be classified as microbial, mechanical, chemical, thermal.
NEED FOR PULP PROTECTION
PULP PROTECTIVE AGENTS
CLASSIFICATION
CAVITY SEALERS: These are materials that provide a protective coating to the walls of the prepared cavity .They are applied to all the walls of the cavity and seal the interface between the restoration and the tooth . Eg: cavity varnish and resin bonding agents.
CAVITY VARNISH: A varnish is a natural gum or a synthetic resin dissolved in an organic solvent . Once it is applied to tooth surface the organic solvent evaporates leaving behind a protective film. Varnish is used beneath amalgam restoration to seal the amalgam tooth interface until corrosion product form to reduce the marginal gap. Thickness of varnish is 2-5 micrometer . They does not provide thermal protection and are contraindicated for GIC .
RESIN BONDING AGENTS: Currently the best method for the bonding composite resin to the tooth structure. Apart form adhesion it also provides cavity sealing. They are also employed for bonding amalgam restorations to reduce micro leakage .
CAVITY LINERS :They are used to provide a barrier against the passage of irritants from the cements or other restorative materials and to reduce the sensitivity of freshly cut dentin . They are usually suspension of calcium hydroxide in a volatile solvent . TYPES : TYPE III GIC , TYPE IV ZOE . Thickness is 0.5 mm
CAVITY BASES: A base is a layer of cement placed beneath the permanent restoration to encourage recovery of the injured pulp and to protect it against numerous types of insults. TYPES : high strength bases and low strength bases .
HIGH STRENGTH BASES provide thermal protection for pulp and mechanical support for the restoration . Eg : zinc phosphate , zinc polycarboxylate, RMGI, GIC
LOW STRENGTH BASES have minimum strength and rigidity . act as a barrier to irritation , chemicals and to provide therapeutic effect to pulp.Eg calcium hydroxide . ZnOE .
REFERENCE : STURDEVANT’S 7TH EDITION
ASHTINDER 🖊

SOURCE- RAMYA RAGHU AND STUDERVANT TEXTBOOK