Abrasion is the pathological wearing away of tooth substance through some abnormal mechanical process. Abrasion usually occurs on the facial surface of the crown and the exposed root surfaces of teeth, but under certain circumstances it may be seen elsewhere such as on incisal or on proximal surfaces.

- Etiology
- Abrasivedentifrices—useofabrasivedentifricescanleadto abrasion of the incisal surface.
- Habitual—Habitualpipesmokermaydevelopabrasion on the incisal edges of lower and upper anterior teeth. In some cases habitual opening of bobby pins may lead to abrasion.
- Horizontal tooth brushing—horizontal tooth brushing may lead to abrasion of the cervical area of teeth.
- Occupational—itoccurswhenobjectsandinstrumentare habitually held between the teeth by people during working. Holding nails or pins between teeth e.g. in carpenters, shoemakers or tailors.
- Dentalflossortoothpicksinjury—improperuseofdental floss and tooth picks.
- Ritual abrasion—it is mainly seen in Africa.Clinical featuresTooth brush injury
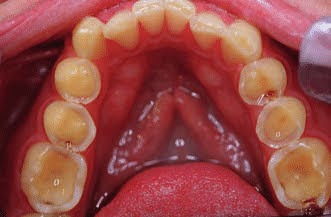
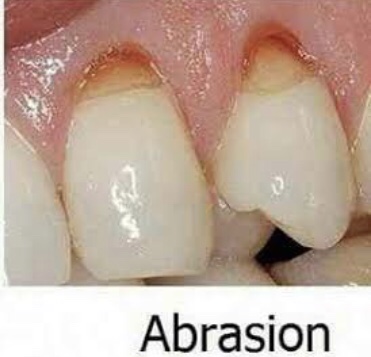
• Sites—itusuallyoccursonexposedsurfacesofrootsofteeth. It is more commonly seen on left side of right handed persons and vice versa.
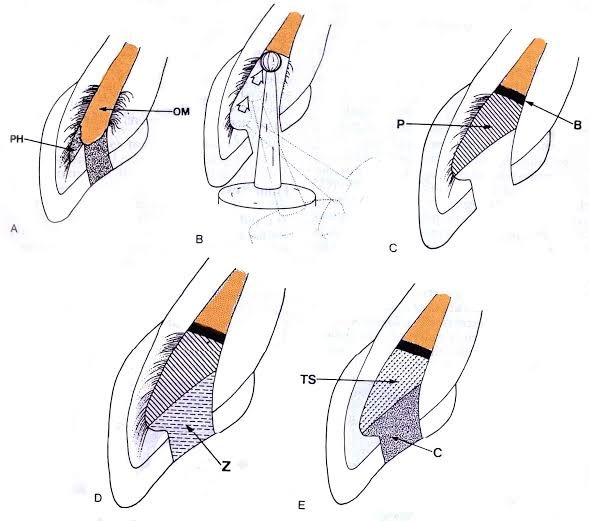
• Mechanism—it occurs due to back and forth movement of brush with heavy pressure causing bristles to assume wedge shaped arrangement between crown and root.
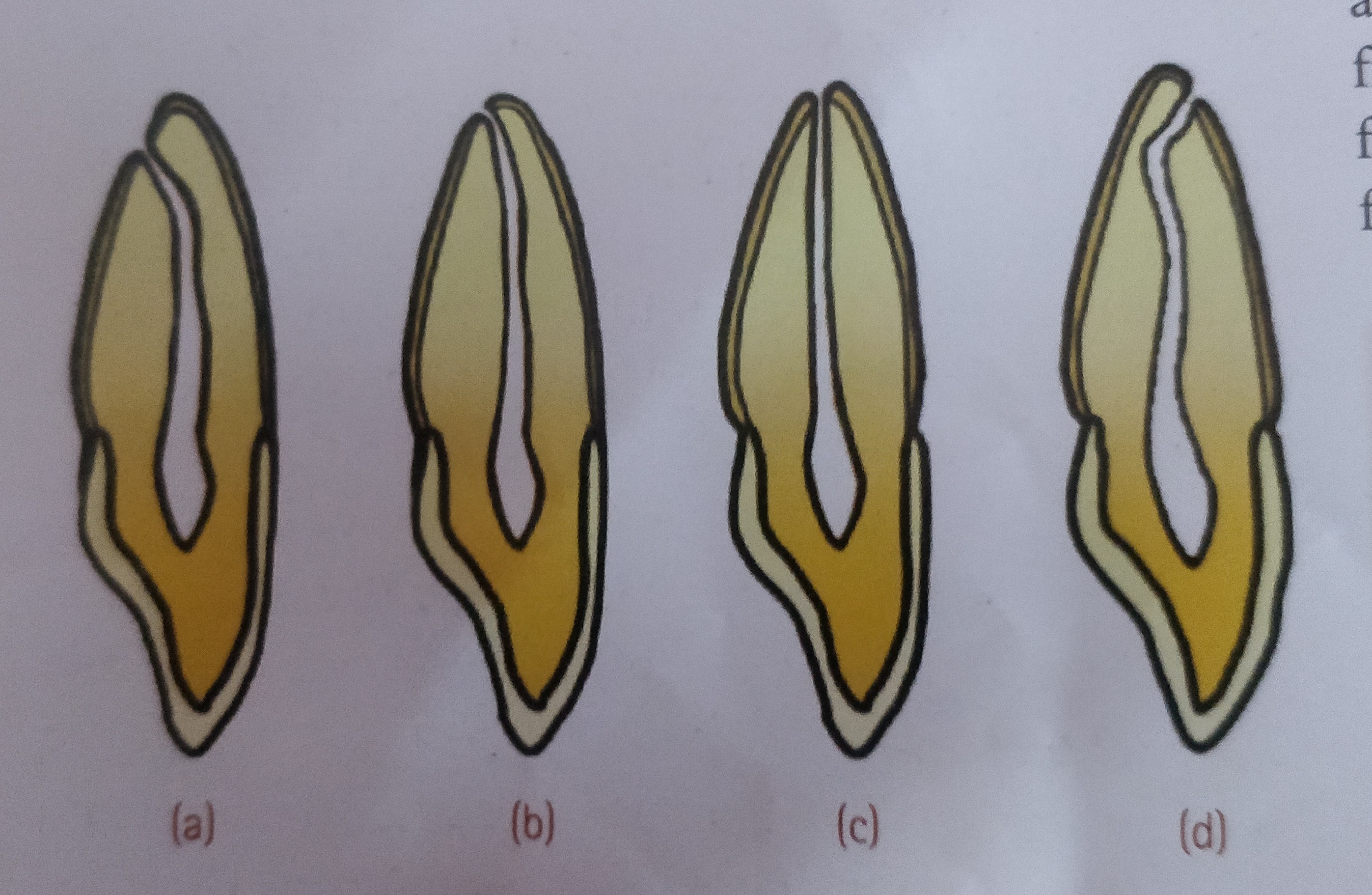
• Appearance—in horizontal brushing there is usually a ‘V’ shaped or ‘wedge’ shaped ditch on the root at cementoenamel junction . It is limited coronally by enamel.
• Symptoms—patient develops sensitivity as dentin becomes exposed.
• Signs—the angle formed in the depth of the lesion as well as that of enamel edge is a sharp one. Cervical lesions caused purely by abrasion have sharply defined margins and a smooth, hard surface. The lesion may become more rounded and shallow, if there is an element of erosion present.
• Dentinal features—exposed dentin appears highly polished Exposure of dentinal tubules and consequent irritation of the odontoblastic processes stimulates secondary dentin formation which is sufficient to protect the pulp from clinical exposure.
Dental floss or tooth pick injury
• Site—Cervical portion of proximal surfaces ,just above the gingival margin, is affected. Grooves on distal surface are deeper than on mesial surface
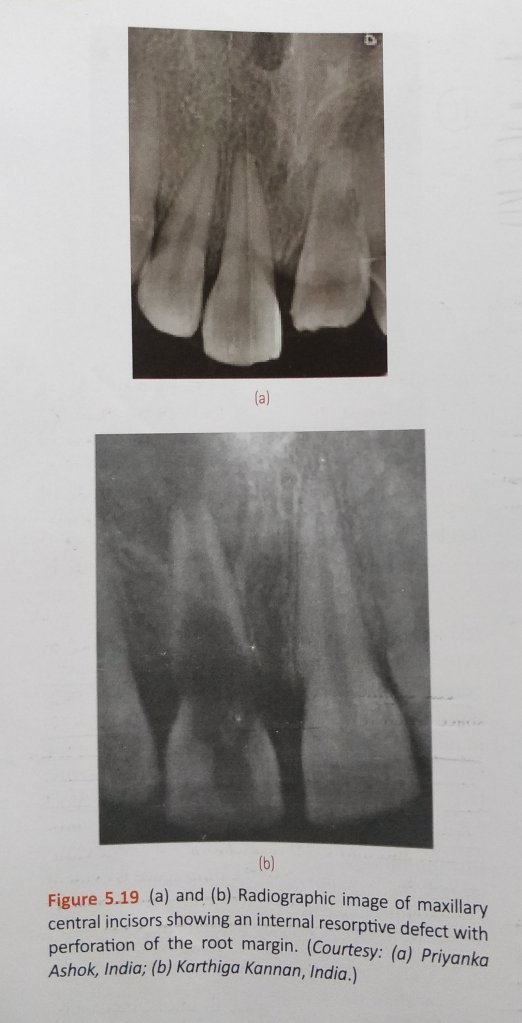
Radiographic features
Tooth brush injury
- Location—radiolucent defect at the cervical level of teeth.
- Shape—well defined semilunar shape ,with borders of increasing density.
- Pulp—pulp chamber may be partially or fully sclerosed in severely affected teeth.Dental floss injury
• Appearance—narrow semilunar grooves in theinterproximal surfaces of teeth near cervical area. - Management
• Modified teeth cleaning habits—modification of teeth cleaning habits will be indicated.
• Removal of cause—elimination of causative agent should be carried out.
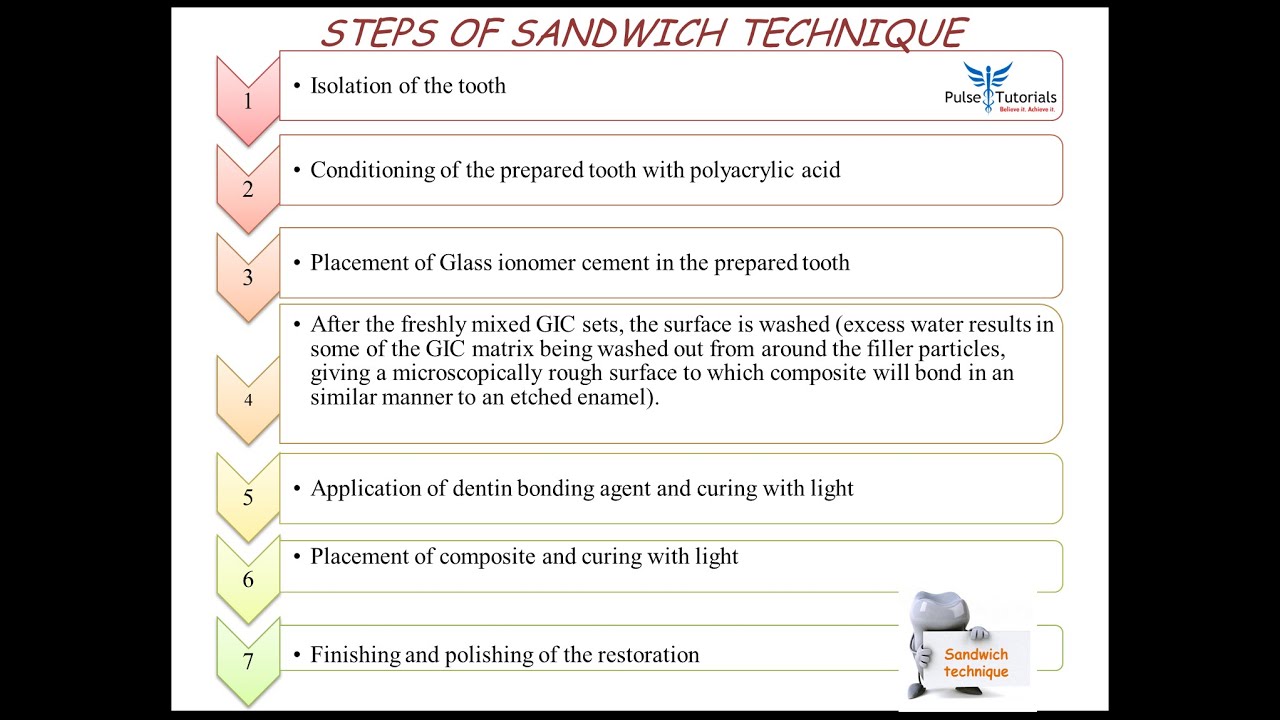
• Restoration—restoration should be done for esthetics purpose and to prevent further tooth wear.
REFERENCE- ANIL GHOM TEXTBOOK OF ORAL MEDICINE [2nd ed]