Examination of neck nodes is important, particularly in head and neck Malignancies and a systematic approach should be followed.Neck nodes are better palpated while standing at the back of the patient. Neck is slightly flexed to achieve relaxation of muscles.
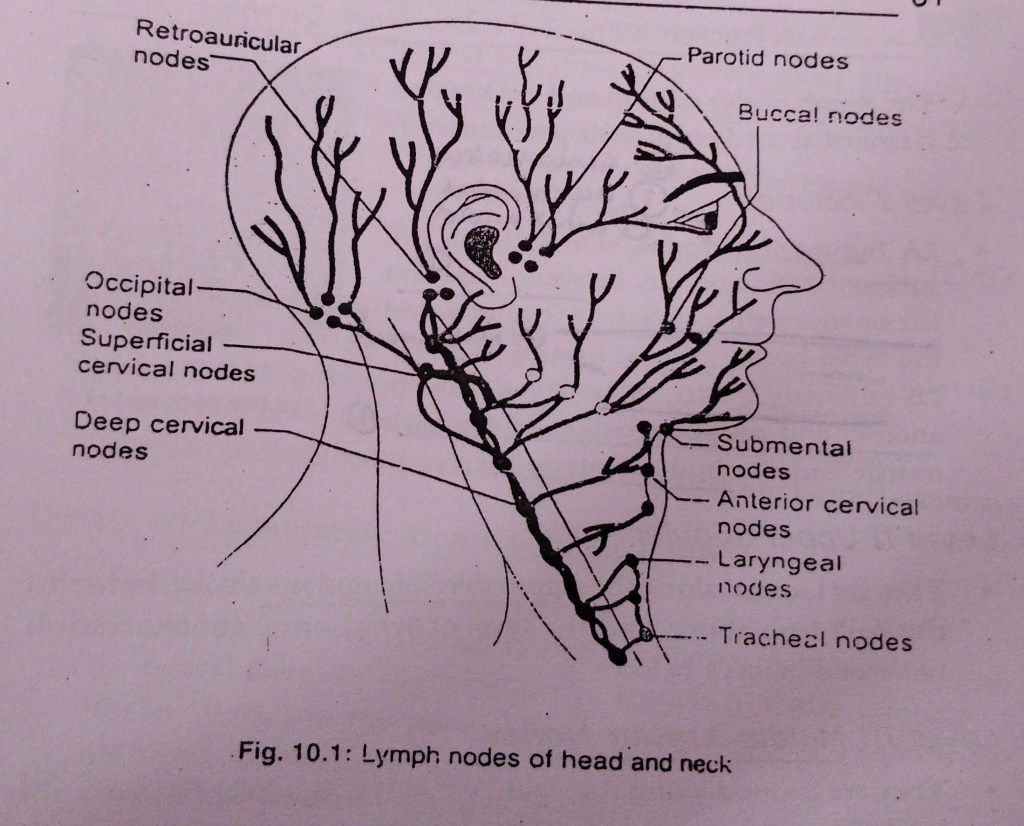
Lymph nodes of head and neck region are classified according to their position level:
- Level I includes :
- IA Submental nodes , which lie in the Submental triangle, i.e between right and left anterior bellies of diagastric muscles and the hyoid bone.
- IB Submandibular nodes , lying between anterior and posterior bellies of diagastric muscle and the body of mandible.
- Level II Upper jugular nodes :
They are located along the upper third of jugular vein, i.e between the skull base above and the level of hyoid bone ( or bifurcation of carotid artery ) below.
- Level III Middle jugular nodes :
They are located along the middle third of jugular vein , from the level of hyoid bone above, to the upper border of cricoid cartilage.
- Level IV Lower jugular nodes :
They are located along the lower third of jugular vein , from upper border of cricoid cartilage to the clavicle.
- Level V Posterior cervical group :
They are located in the posterior triangle ,i.e between posterior border of sternocleidomastoid ( anteriorly ) , anterior border of trapezius ( posteriorly ) , and the clavicle below. They include lymph nodes of spinal accessory chain , transverse cervical nodes and supraclavicular nodes.
- Level VI Anterior compartment nodes :
They are located between the medial borders of sternocleidomastoid muscles ( or carotid sheath ) on each side, hyoid bone above and suprasternal notch below. They include prelaryngeal, pretracheal , paratracheal nodes .
- Level VII :
They are located below the suprasternal notch and include nodes of the upper mediastinum.
Examination of various lymph nodes:
- Submental nodes : Roll the fingers below the chin with patients head tilted forward.
- Submandibular nodes : Roll your fingers against inner surface of mandible with patients head gently tilted on one side.
- Parotid ( preauricular ) nodes : Roll your fingers in front of the ear , against the maxilla .
- Postauricular ( mastoid ) nodes : Roll the fingers behind the ears.
- Internal jugular chain : Examine the upper , middle and lower groups. Many of them lie deep to sternomastoid muscle which may need to be displaced posteriorly.
- Transverse cervical nodes
- Supraclavicular ( scalene ) nodes : Roll your fingers gently behind the clavicles.
A normal lymph node cannot be felt. If a node is palpable, it must be abnormal.
Area of lymphatic drainage of face :
The face has 3 lymphatic territories :
- The upper territory : Including the greater part of the forehead, the lateral halves of the eyelids, the conjunctiva, the lateral part of the cheek and the parotid area, drains into the preauricular (parotid) nodes.
- The middle territory : Including a strip over the median part of the forehead, the external nose, the upper lip, the lateral part of the lower lip, the medial halves of the eyelids, the medial part of the cheek and the greater part of the lower jaw, drains into the Submandibular nodes.
- The lower territory : Including the central part of the lip and chin, drains into the Submental nodes.
References:
A practical manual of Public Health Dentistry by CM Marya.
Written by - Dr.Urusa I Inamdar
- Anatomy
- Bacteria
- Biochemistry
- Cardiovascular System
- Conservative Dentistry And Endodontics
- Dental Antomy
- Dental Histology
- Dental Materials
- Embryology
- EXCLUSVIVE INTERVIEW
- Gastrointestinal System
- General Medicine
- General Surgery
- Hematology
- Histology
- Immune Response & Autoimmune Disorders
- Microbiology
- Mnemonic
- Musculoskeletal
- Neurological Pathologies
- Neurosciences
- Oral And Maxillofacial Surgery
- Oral Medicine And Radiology
- Oral Pathology
- orthodontics
- Pathology
- PCC
- PCP
- Pedodontics
- Periodontology
- Pharmacology
- Physiology
- Picture Based Questions
- prosthodontics
- Public Health Dentistry
- PYQs of AIIMS/PGI
- Renal System
- Research
- Respiratory System
- Review Series
- Special Senses
- Uncategorized