Name suggested by Willis.
Most common neoplasm of salivary gland tumor.
Benign neoplasm- consisting of cells exhibiting the
ability to differentiate to epithelial (ductal and
nonductal) cells and mesenchymal (chondroid,
myxoid, osseous) cells.
Other names:
- Branchioma,
- enclavoma,
- teratoma,
- cyindroma,
- myxochondrocarcinoma.
Salivary gland tumor origin: EPITHELIAL
Shows cytogenic abnormalities in chomosomes- 12q13-15.
Putative pleomorphic adenoma gene(PLAG1) has been
mapped to chromosomes 8q12
Histogenesis:-
- Currently, numerous theories centre around the myoepithelial cell and the reserve cell in the intercalated duct.
- Ultrastructural studies have confirmed the presence of both ductal and myoepithelial cells in pleomorphic adenomas.
- It follows that possibly either or both may play active roles in the histogenesis of the tumour.
- Hubner and his associates:- have postulated that the myoepithelial cell is responsible for the morphological diversity of the tumour, including the production of the fibrous, mucinous, chondroid and osseous areas.
- Regezi and Batsakis:- postulated that the intercalated duct reserve cell can differentiate into ductal and myoepithelial cells, and the latter, in turn, can undergo mesenchymal metaplasia, since they inherently have smooth muscle-like properties. Further differentiation into other mesenchymal cells then can occur.
- Batsakis:- has discussed salivary gland tumourigenesis, and while still implicating the intercalated duct reserve cell as the histogenetical precursor of the pleomorphic adenoma, stated that the role of the myoepithelial cell is still uncertain and that it may be either an active or a passive participant histogenetically.
- Finally, Dardick and his associates have questioned the role of both ductal reserve and myoepithelial cells. They stated that a neoplastically altered epithelial cell with the potential for multidirectional differentiation might be histogenetically responsible for pleomorphic adenoma.
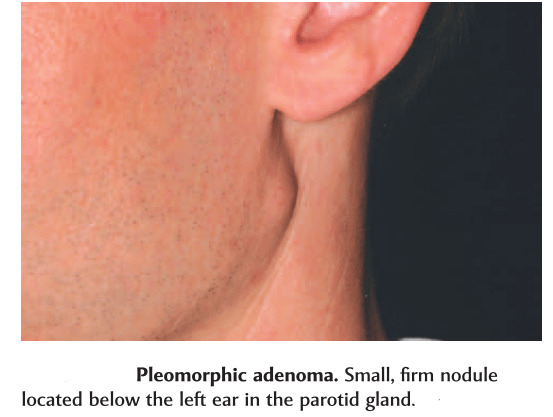
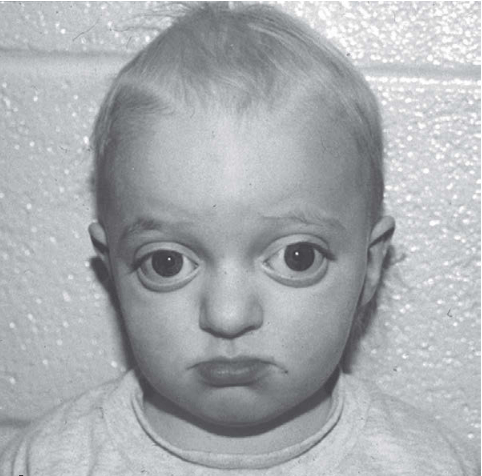
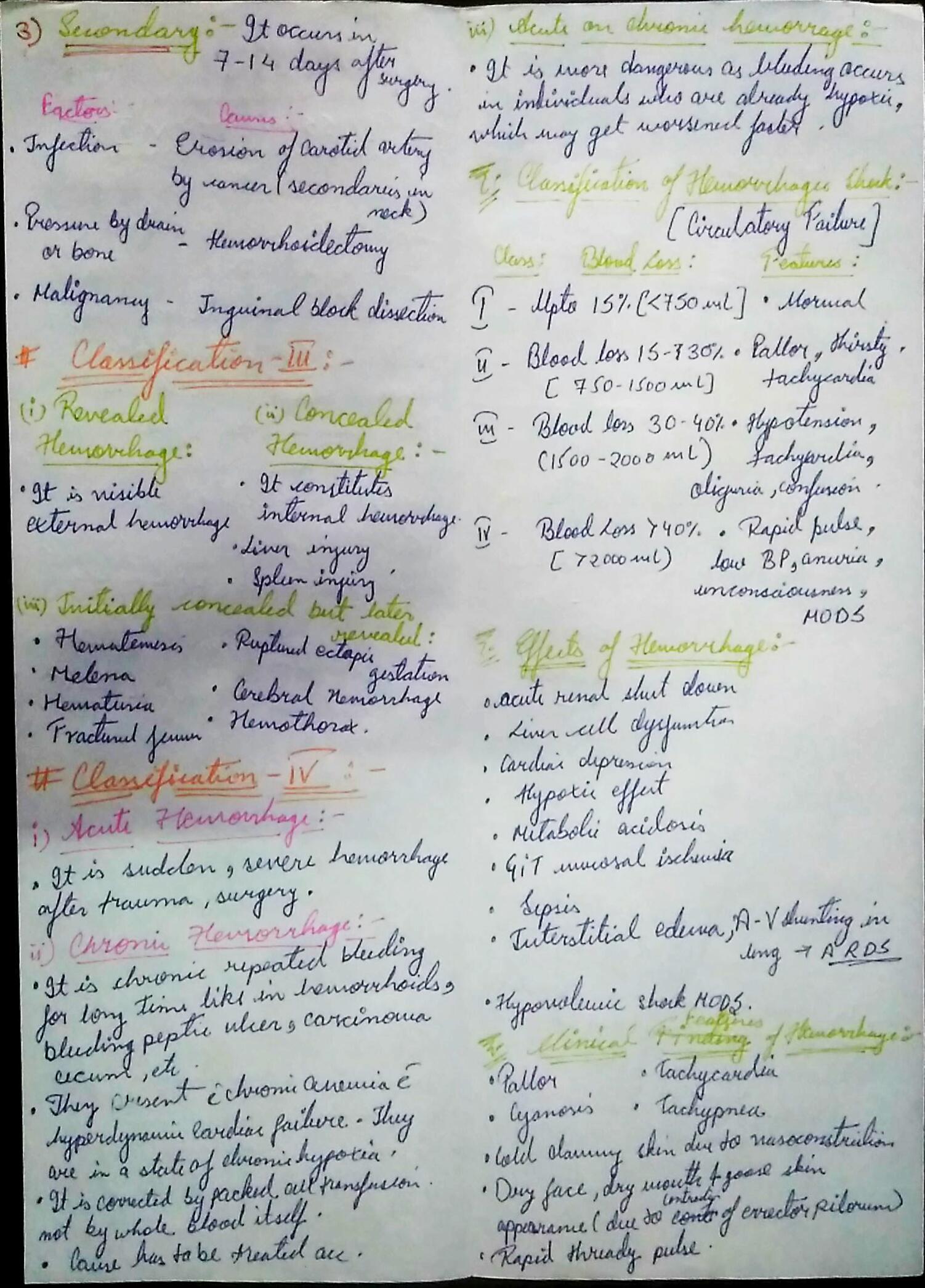
CLINICAL FEATURES:-
Most common tumor.
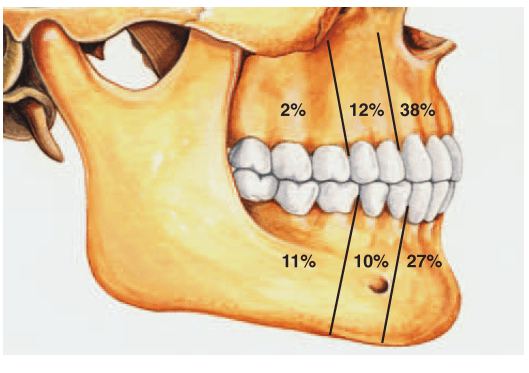
Rate of occurance: 60-70%- parotid glands
40-60%- submandibular glands
40-70%- minor salivary glands
seldomly- sublingual glands
Age: 30-50 years
Sex: female> male – 3:1 – 4:1
In parotid- presents in the lower lobe of the superior lobe
as a mass over the angle of the mandible, below and infront
of the ear.
Clinical presentation: painless, slow growing, firm
mass, initially small in size and begins to increase in
size.
Initially movable but with continued growth become
more nodular and less movable.
Recurrent tumor- multinodular, fixed on palpation.
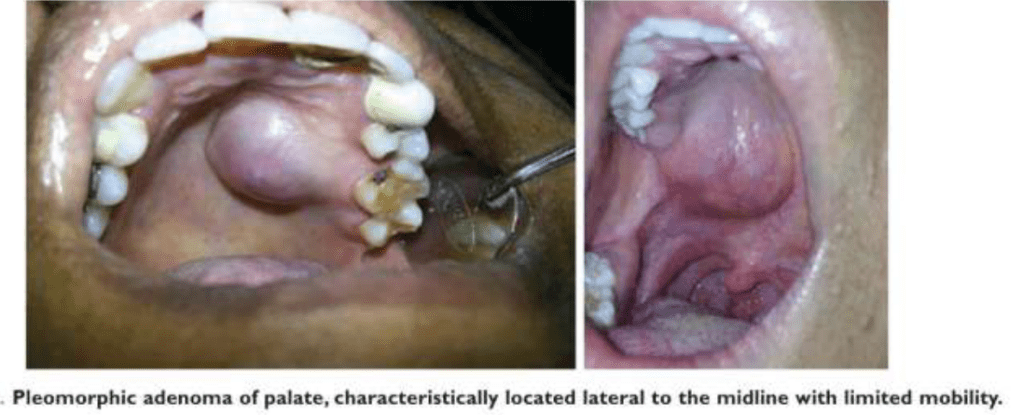
Palate – intraorally common site.
Seldom ulcerated- unless secondarily traumatized.
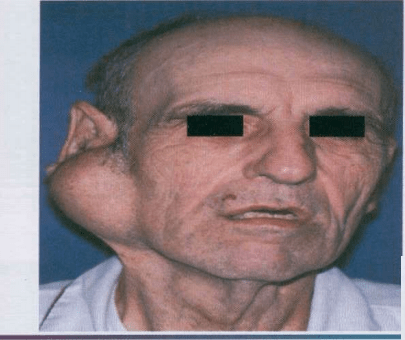
The parotid gland.
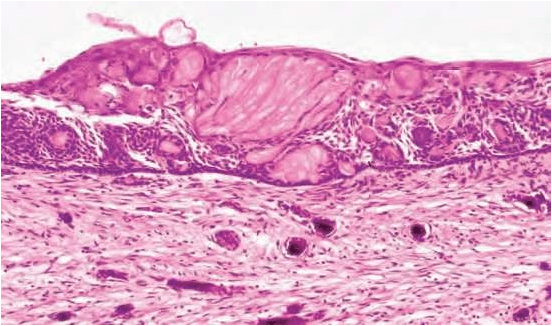
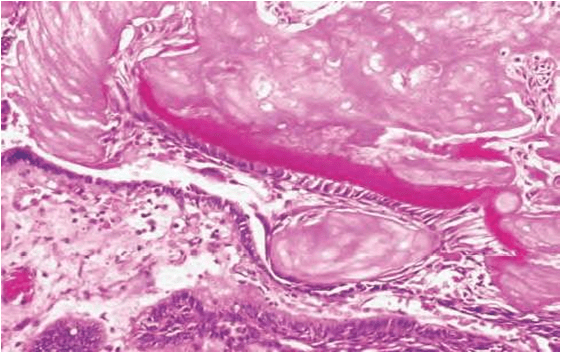
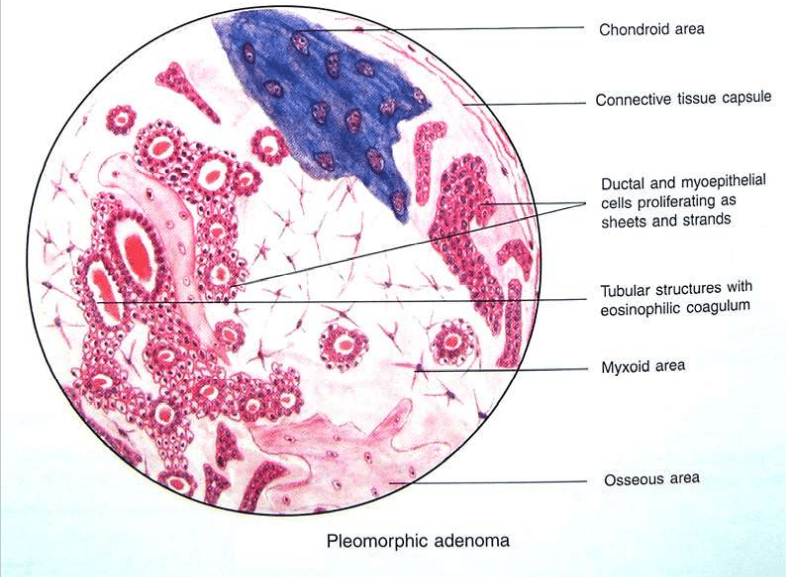
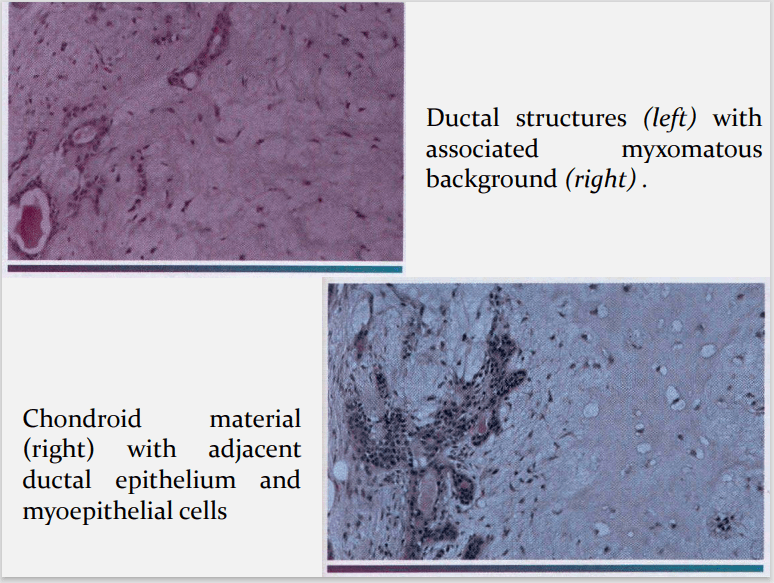
HISTOPATHOLOGY:-
HALLMARK: Morphologic Diversity.
Charecterized by- Variable, Diverse, Structural & histologic
patterns.
It demonstrate glandular epithelium and mesenchyme like
tissue and the proportion of each component varies widely.
Typically a well-circumscribed encapsulated tumor
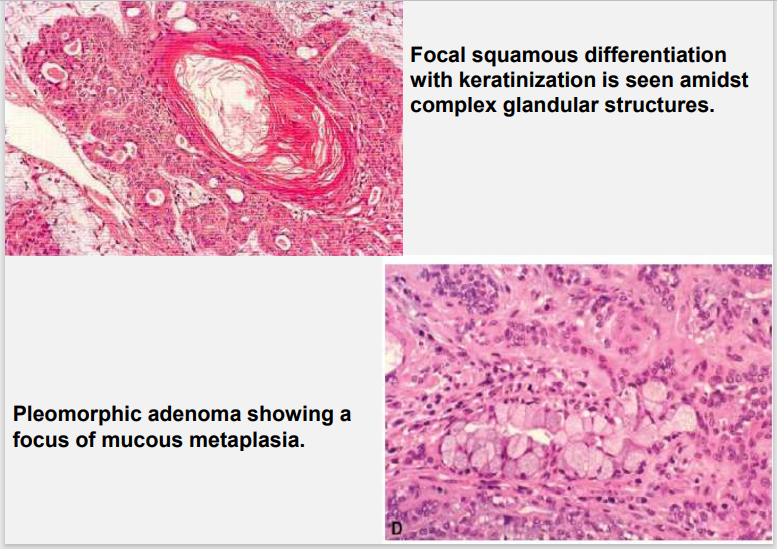
The epithelium often forms ducts and cystic structures or may
occur as islands or sheets of cells , anastomosing cords and foci
of Keratinizing squamous cells and spindle cells .
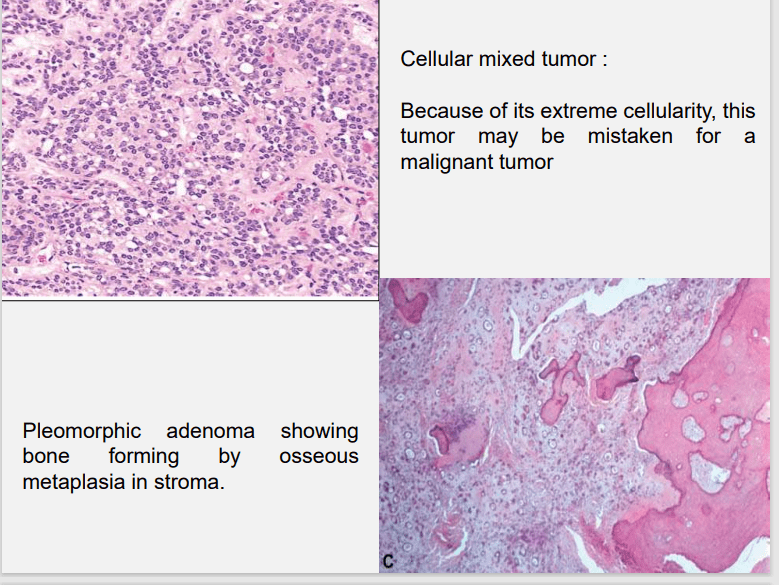
- Foote and Frazell (1954) categorized PA into:
a) Primarilly myxoid (36%)
b) Myxoid and cellular component in equal proportions
(30%)
c) Predominantly cellular (22%)
d) Extremely cellular (12%)
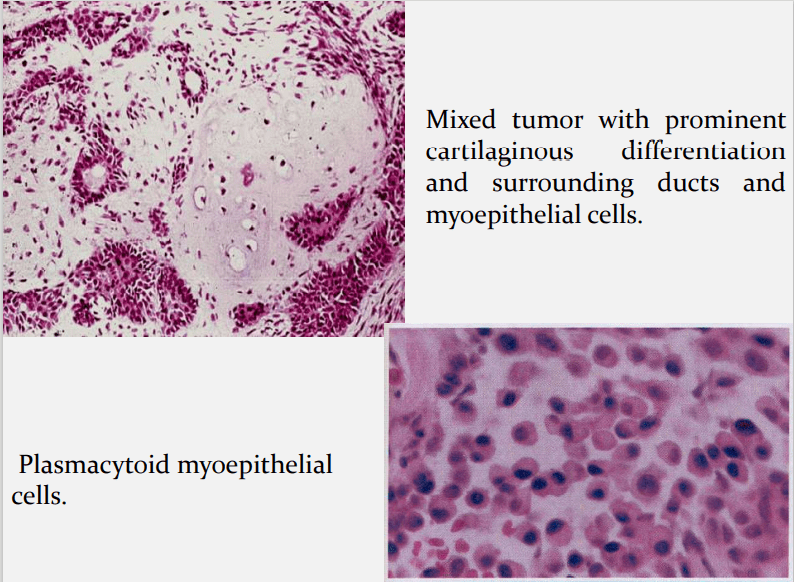
Myoepithelial cells are major component of PA.
Have variable morphology- sometimes appearing as
angular or spindled, some with eccentric nucleus
resembling plasma cells.
Are responsible for characteristic mesenchyme like
changes.
Vacuolar degeneration of myoepithelial cells can produce a
chondroid appearance.
the stroma exhibits areas of an eosinophilic hyalinized change,
fat or osteoid also is seen.
DIFFIRENTIAL DIAGNOSIS:-
Polymorphous low grade adenocarcinoma, PLGA
Adenoid cystic carcinoma, AdCC
Epithelial myoepithelial carcinoma, EMC
Squamous cell carcinoma, SCC
Mucoepidermoid carcinoma, MEC
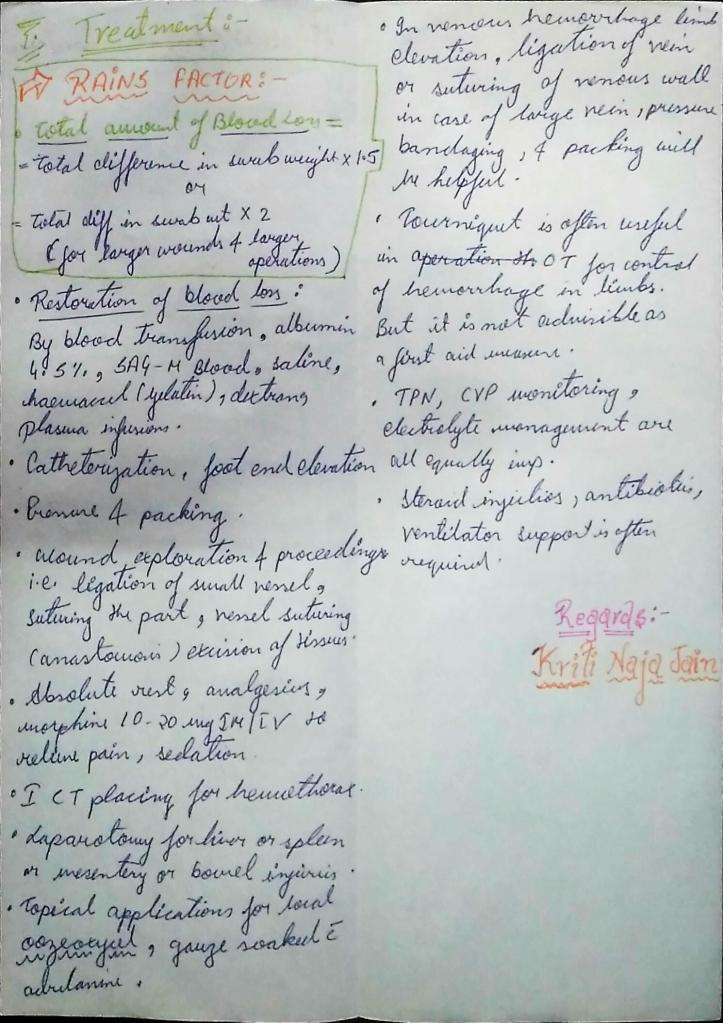
TREATMENT:-
Surgical excision
Superficial parotidectomy with preservation of the facial nerve
Local enucleation should be avoided – resulting in seeding of
the tumor bed.
Deep lobe of the parotid- total parotidectomy is usually
necessary also with preservation of the facial nerve.
Submandibular tumors – Total removal of the gland with the
tumor.
Malignant degeneration is a potential complication, resulting in
a carcinoma ex pleomorphic adenoma.
The risk of malignant transformation is probably small, but it
may occur in as many as 5% of all cases.
REFERENCES:-
1.Shafers- 8e
2.Nevill’s-3rd e
3.Maji Jose
4.GOOGLE Images