Wegener’s granulomatosis is a disease of unknown aetiology, which basically involves the vascular, renal and respiratory systems. It involves the nose, paranasal air sinuses, lower respiratory tract, gut, joints, nervous system, and kidneys. Involvement of the kidney is the common cause of death.
This disease is caused by an abnormal immune reaction secondary to a nonspecific infection or a hypersensitivity reaction to an unknown antigen.

Clinical Features
>Wegener’s granulomatosis may occur at any age, although the majority of cases are in the fourth and fifth decadesof life.
>There is a slight predilection for occurrence in males.
>It is best described as a multisystem disease, which is usually first characterized clinically by the development of rhinitis, sinusitis, and otitis or ocular symptoms.
>The patient soon develops a cough and hemoptysis as well as fever and joint pain.
>Hemorrhagic or vesicular skin lesions are also commonly present.
>Granulomatous lesions of the lungs are found on the chest radiograph, while the glomerulonephritis, which develops ultimately, leads to uraemia and terminal renal failure.
>In nervous system, sensory neuropathy may be an occasional finding.
>Prognosis—the disease is usually fatal, with mean survival time of 5 months. Death occurs due to involvement of kidney.
Oral Manifestations
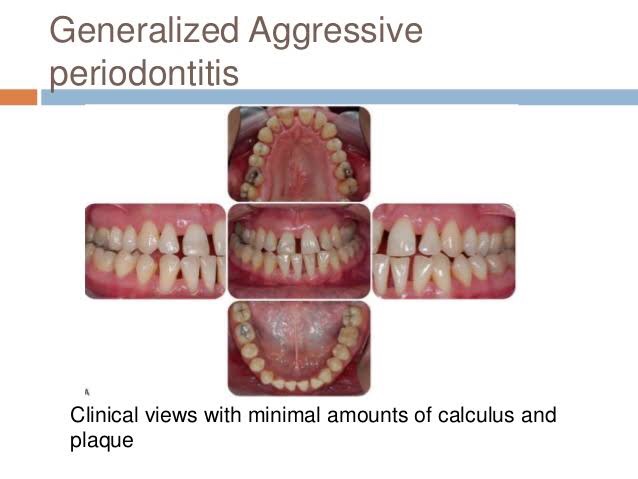
Involvement of the gingiva has been the most common and characteristic manifestation, and is termed as strawberry gingivitis.Gingival lesions may manifest as ulcerations, friable granular lesions, or simply enlargements of the gingiva.
The inflammatory process starts in the interdental papilla and spreads rapidly to the periodontal structure and leads to bone loss and tooth mobility.
Palate—orallesionstypicallyincludeulcerationofthe palate by extension of nose lesions and destruction of nasal septum. This will lead to perforation of palate.
• Teeth—theremaybelooseningofteethwithinsomecases spontaneous exfoliation. After extraction of teeth patient is usually noticed poor healing.

Laboratory Findings
Laboratory findings include anaemia, leukocytosis, elevated erythrocyte sedimentation rate, and hyperglobulinaemia. Because of kidney involvement, haematuria is common, as well as the finding of albumin, casts, and leukocytes in the urine. Circulating immune complexes have been demonstrated in some patients, but this is not a consistent finding.
Histologic Findings
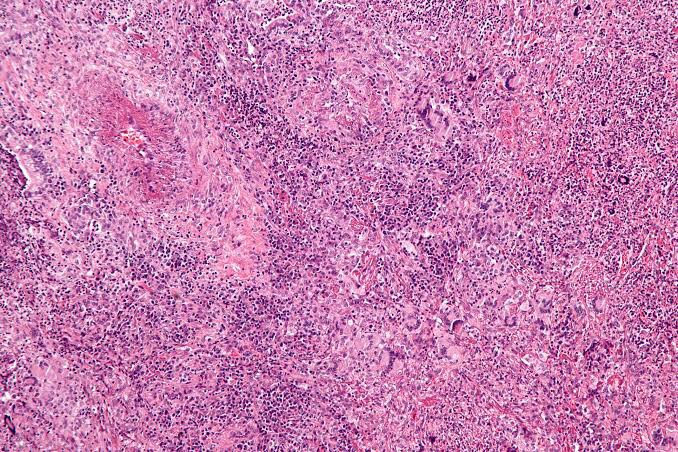
Wegener’s granulomatosis presents a pattern of mixed inflammation centred around the blood vessels.
The lesions in the upper respiratory tract and lungs consist of giant cell necrotizing granulomatous lesions showing vasculitis.
Oral biopsy specimens show pseudoepitheliomatous hyperplasia and subepithelial abscesses. The gingival and other lesions show a nonspecific granulomatous process with scattered giant cells.
Diagnosis
- Clinical diagnosis—typical strawberry gingivitis with necrotic ulceration in the oral cavity.
- Laboratorydiagnosis—cytoplasmiclocalizationispresent with Wegener’s granulomatosis. Histopathologically chronic inflammatory cells and multinucleated giant cells are found.
- Differential Diagnosis
- Agranulocytosis, leukemia, lymphoma—diagnosis by blood picture, possibly histology.
- Management
- Cotrimoxazole—it is combination of trimethoprim and sulfamethoxazole. It has proved to be effective as an adju- vant or sole therapy in both localized and generalized forms.
- Corticosteroids—regimenofcyclophosphamide12mg/ kg body weight/day with prednisolone 1 mg/kg body weight have been utilized to obtain complete remission.
- Others—other treatment modalities includes cyclo- sporine, intravenous pooled immunoglobulin, and local irradiation.
REFERENCE- SHAFER’S TEXTBOOK OF ORAL PATHOLOGY {8TH ED} AND ANIL GHOM TEXTBOOK OF ORAL MEDICINE