If you think orthodontics is only about teeth and jaws, think again.
The temporomandibular joint (TMJ)—especially the glenoid fossa—quietly influences some of the most important facial patterns you diagnose every day:
- Class II retrusion vs. Class III prognathism
- High-angle vs. low-angle growth patterns
- Deep bites, open bites, vertical maxillary excess
- Mandibular rotation direction
And yet, most students rarely analyze the fossa position.
Baccetti et al. (1997) decided to change that.
The Big Question
Does the position of the glenoid fossa differ between Class I, II, III and between high-, normal-, and low-angle facial types?
If yes—can this help us diagnose better?
Spoiler: YES. And the vertical dimension tells a story even more strongly than the sagittal one.
THE STUDY AT A GLANCE
Sample
- 180 children (7–12 years) — equal males/females
- Pretreatment cephalograms
- Clear glenoid fossa outline required
- Divided into 9 subgroups:
- Class I, Class II, Class III
- Low-, normal-, high-angle
- Combined internally for controlled comparison
Why this is important?
Because it removes age/sex bias → differences truly reflect facial type, not growth/sex variation.
What Exactly Did They Measure?
Two planes of interest:
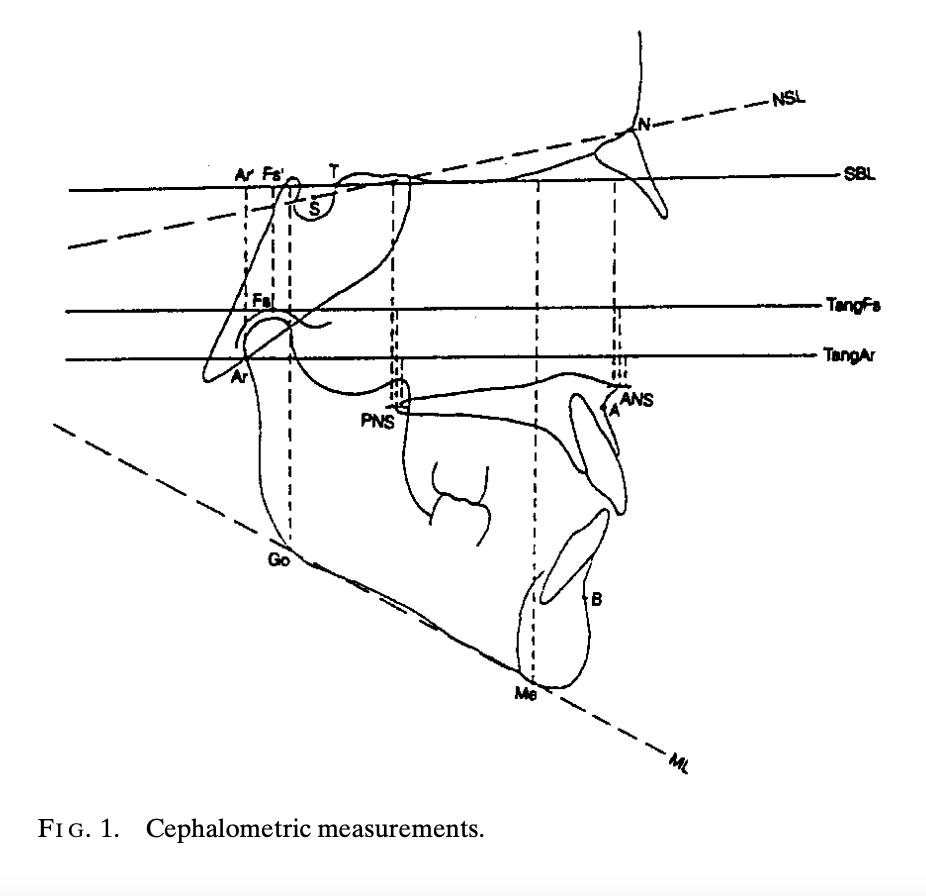
1. Sagittal (Anterior–Posterior) TMJ Position
Key indicators:
- T–Fs’: Distance from sella wall (point T) to fossa summit projection
- T–Ar’: Distance from point T to articulare projection
Shorter distances = fossa positioned more posteriorly.
2. Vertical (Cranial–Caudal) TMJ Position
Key indicators:
- Fs–Fs’
- Ar–Ar’
- TangFs–PNS and TangAr–PNS
- SBL–Me, SBL–Go, SBL–ANS
These measure how high or low the fossa sits relative to the cranial base and nasal spines.
Takeaway:
Vertical indicators tell you far more than sagittal ones.
THE LOGIC OF THE FINDINGS
Let’s break them down so they make intuitive sense.
1. Sagittal Findings (Class I vs II vs III)
Class II → Glenoid Fossa is More Posterior
A posterior fossa places the condyle backward → enhances mandibular retrusion → increases ANB.
This fits what you see clinically:
- Class II often have posteriorly positioned condyles
- Functional appliances can remodel the fossa anteriorly (as noted in prior studies)
Class III → Glenoid Fossa is More Anterior
An anteriorly placed fossa gives the mandible a “forward hinge.”
This contributes to:
- Lower ANB
- Apparent mandibular prognathism
Logical link:
The fossa location magnifies or mitigates jaw relationships.
2. Vertical Findings (Normal vs Low vs High Angle)
This is where the study becomes extremely clinically valuable.
High-Angle Patients → Glenoid Fossa is More Cranial (Higher Up)
A high-positioned fossa elevates the condyle → encourages vertical growth pattern → clockwise rotation → long-face appearance.
Clinical correlation:
- Hyperdivergent faces
- Increased mandibular plane angle
- Open bite tendencies
- Posterior rotation of mandible
Low-Angle Patients → Glenoid Fossa is More Caudal (Lower Down)
A low-positioned fossa → condyle sits lower → reduces vertical dimension → promotes horizontal growth.
Clinical correlation:
- Short face
- Deep bite tendencies
- Strong chin
- Forward mandibular rotation
And the most important part:
The posterior nasal spine (PNS) is an excellent reference point for evaluating fossa height.
VERTICAL > SAGITTAL
The authors emphasized that vertical differences were more pronounced, more consistent, and more diagnostically useful than sagittal differences.
This means:
If you want to understand a patient’s growth pattern and mandibular rotation tendencies, analyze fossa height.
Clinical Logic — Why Does Fossa Position Matter?
Understanding fossa position helps you answer critical orthodontic questions:
A. Why does a patient grow clockwise vs counterclockwise?
High fossa = clockwise rotation (high-angle)
Low fossa = counterclockwise rotation (low-angle)
B. Why do some Class II patients look worse even after camouflage?
Because a posterior fossa inherently pushes the mandible back.
C. Why do functional appliances work better in some children?
Certain fossa shapes/positions favor forward condylar adaptation.
D. Why are some deep bites so stubborn?
Low-angle → low fossa → strong masticatory musculature → deep bite tendency.
Key Cephalometric Pearls You Should Remember
1. Class II = posterior fossa
2. Class III = anterior fossa
3. High-angle = high fossa
4. Low-angle = low fossa
5. Vertical position is the best diagnostic clue
Practical Clinical Use (Student Cheat Sheet)
If you see a HIGH-ANGLE face…
Expect:
- High fossa
- Clockwise rotation
- Weak chin
- Open bite risk
- Need for vertical control
If you see a LOW-ANGLE face…
Expect:
- Low fossa
- Counterclockwise rotation
- Strong chin
- Deep bite risk
- Avoid excessive uprighting/extrusion of molars
If you see a CLASS II face…
Check:
- Is the fossa posterior?
- Is the retrusion skeletal or positional?
If you see a CLASS III face…
Check:
- Is the mandible truly prognathic?
- Or is the fossa anteriorly placed?
Why This Study Matters Today (Even in CBCT Era)
Although the study used 2D cephalograms, the concept is timeless:
TMJ position is not the result of teeth; it helps shape the face.
Understanding fossa position allows you to predict growth and plan treatment wisely.
Today, CBCT gives even clearer visualization—but the same principles apply.
Final Takeaway for Ortho Students
If you understand this one idea, you have mastered the essence of the paper:
The glenoid fossa is not a passive socket—it actively influences sagittal and vertical facial patterns.
Its position helps determine whether a patient grows long, short, forward, or backward.
Once you learn to read it, the TMJ becomes one of your most powerful diagnostic tools.
