Class III cases can be tricky—because what you see clinically may not always be what’s truly happening skeletally.
A major reason for this confusion is the mandibular closure path.
In simple terms, you must ask:
👉 Does the mandible really sit forward?
or
👉 Is it just sliding forward because the incisors collide during closure?
This distinction is essential for correct diagnosis and avoiding overtreatment.
True vs Pseudo Class III — The Core Difference
| Feature | True Class III 😬 | Pseudo Class III 🙂 |
|---|---|---|
| Cause | Skeletal discrepancy | Premature incisor contact |
| Forward mandibular shift | ❌ Minimal / None | ✅ Present (functional slide) |
| Ceph ANB | Negative due to skeletal | Improves when edge-to-edge |
| Profile | Concave | Straight / near normal |
| Treatment | Growth modification / Surgery | Remove interference + limited ortho |
Why Functional Shifts Matter So Much
A patient may appear severely Class III when teeth are in habitual occlusion.
But once you guide them into edge-to-edge, the face and ceph often tell a different story.
This happens because many Class III patients have a:
Functional forward mandibular displacement
Also described as:
- forward displacement
- functional protrusion
- anterior slide
- mandibular slide
🦷 Premature incisor contact → Mandible slides forward → Posterior teeth finally occlude
This functional shift can exaggerate the skeletal discrepancy and lead to misdiagnosis.
The closure path also involves a vertical component. As the mandible moves forward, it may also rotate downward, further altering the apparent skeletal relationship
What Actually Happens During Closure (Based on the Study)
1. Closure begins → incisors touch edge-to-edge
→ This causes an initial forward shift of the mandible.
2. As closure continues → condyles move backward
→ This cancels most of the forward movement.
3. Final result
✅ Most Class III patients show little to no real mandibular displacement when the posterior teeth are in occlusion.
This means the apparent Class III worsening is mostly positional, not skeletal.
Role of Overbite in the Functional Shift
Overbite depth determines how much shift can happen:
Deep overbite
➡️ Less functional forward displacement
➡️ Hinge closure pushes condyles backward effectively
Shallow overbite
➡️ More chance of a genuine functional slide
➡️ Slight displacement may persist even in full occlusion
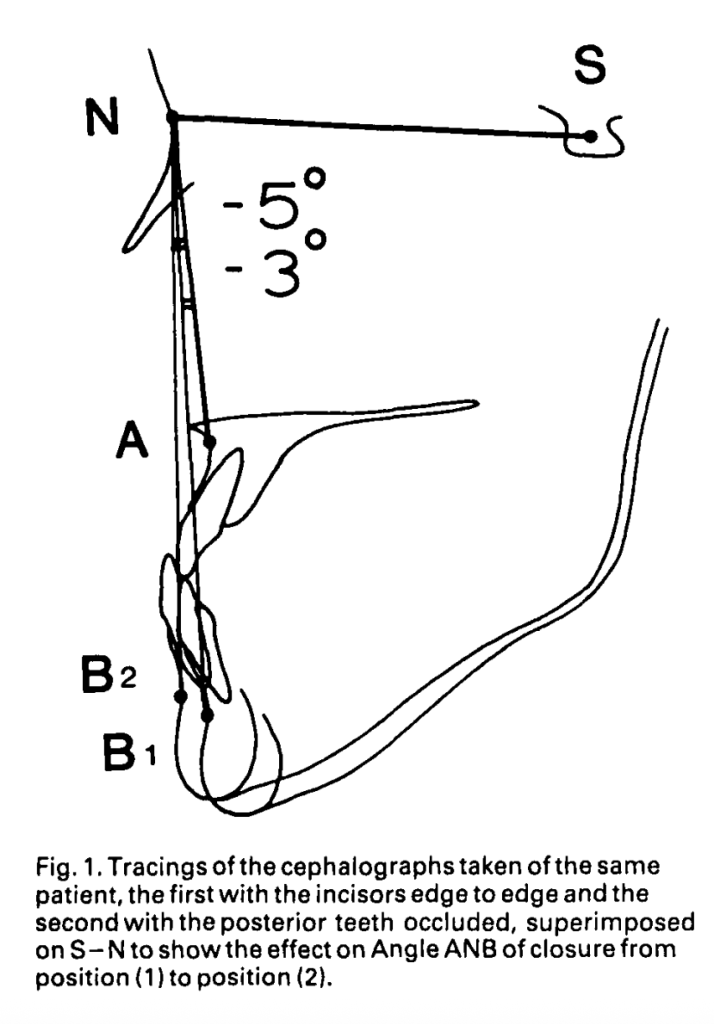
What Two Cephs Really Tell You
Taking both:
- Edge-to-edge ceph, and
- Habitual occlusion ceph,
usually does not dramatically change your skeletal assessment.
Typical Changes Seen
| Parameter | Edge-to-edge | Habitual Occlusion | Interpretation |
|---|---|---|---|
| SNB | ↓ by ~3° | ↑ | Hinge closure effect, not forward displacement |
| ANB | ↑ by ~3° | ↓ | Mostly due to vertical change from overbite |
Key insight:
The ANB difference is largely due to vertical position changes—not true mandibular forward movement.
When Does Residual Functional Shift Still Matter?
For most patients → minimal to none.
But in patients with shallow overbite (<4 mm) a small functional shift may be measurable:
- SNB decreases slightly (≈ –0.4°)
- ANB increases slightly (≈ +0.28°)
These differences are statistically significant, but rarely large enough to alter your diagnosis.
Practical Chairside Screening
A. Suspect Pseudo-Class III if:
- A noticeable forward jump during closure
- Edge-to-edge looks less Class III
- Shallow overbite
- Strong anterior interferences
B. Suspect True Skeletal Class III if:
- No forward shift on closure
- Edge-to-edge still looks Class III
- Deep overbite (hinge movement dominates)
- Minimal ceph difference between both positions
Should You Take Two Cephs?
According to the study:
❗ Routine second ceph is not necessary in most cases.
Habitual occlusion ceph is usually sufficient because:
- The functional slide is often neutralized during full closure.
- Skeletal interpretation remains largely unchanged.
✔ Use a second ceph only when evaluating a suspected functional shift.
Quick Exam Tips
- When asked about functional mandibular slide in Class III, emphasize rotation vs. translation.
- Remember the relationship between overbite depth and angular changes.
- Understand the clinical implications of study results: Use edge-to-edge ceph only when absolutely necessary.
- For cephalometric interpretation, ANB changes can be influenced by vertical mandibular rotation.
- Be able to describe how mandibular closure path affects ceph interpretation.
