Primary stability and safety for palatal TADs depend on two anatomic variables: overall bone depth (BD) to avoid nasal perforation and cortical bone thickness (CBT) to achieve adequate insertion torque and stability. BD and CBT vary systematically across the palate, so site choice—not just screw design—drives success and risk mitigation in everyday mechanics.
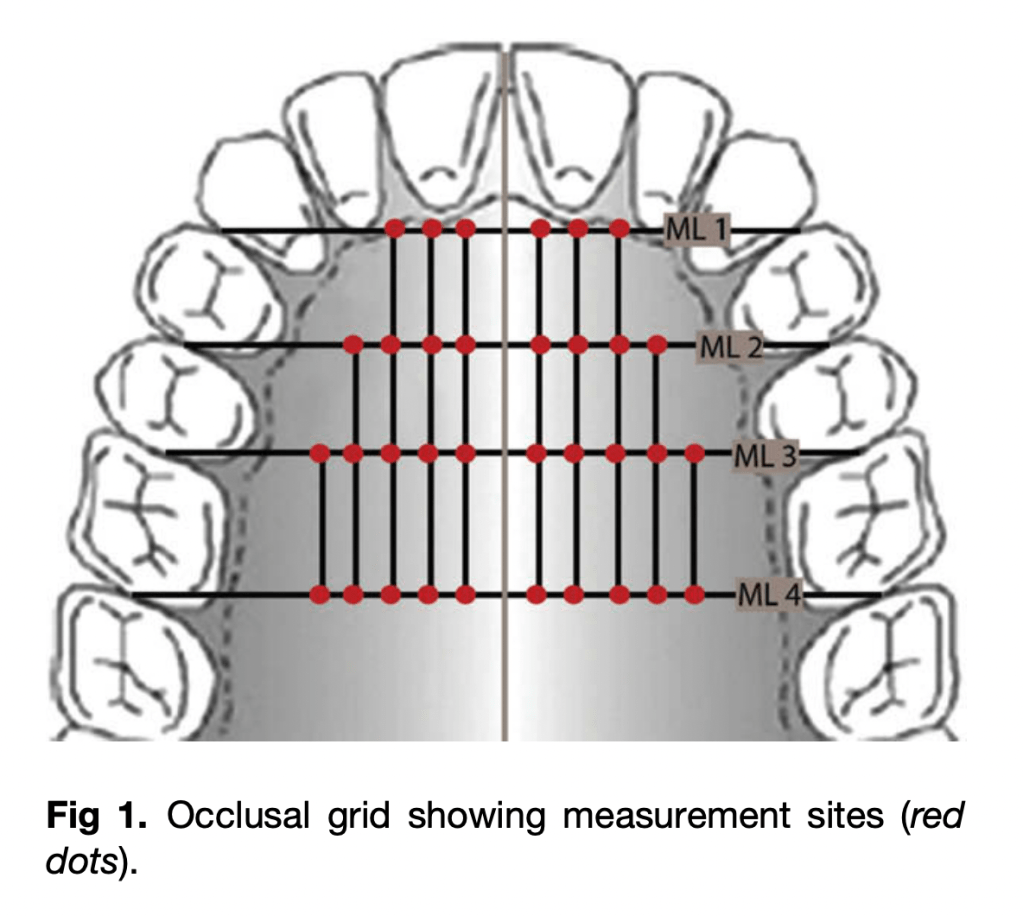
Measurement Levels (MLs)
- ML1: Canine–1st premolar
- ML2: 1st–2nd premolars
- ML3: 2nd premolar–1st molar
- ML4: 1st–2nd molars
Key Principles
- Bone Depth (BD): Greatest in anterior palate, decreases posteriorly.
- Cortical Bone Thickness (CBT): Highest anteriorly, decreases posteriorly.
- Primary Stability: Requires CBT > 1 mm for acceptable success.
- Safe Implant Length:
- Anterior (ML1 & ML2): 6–8 mm implants generally safe.
- Posterior (ML3 & ML4): Risk of nasal perforation if ≥6 mm fully seated.
Bone Depth (BD) – Mean values (mm)

| Level (ML) | 2 mm | 4 mm | 6 mm | 8 mm | 10 mm | Zone |
|---|---|---|---|---|---|---|
| ML 1 | 8.7 | 7.6 | 7.3 | — | — | 🟢 |
| ML 2 | 8.7 | 8.0 | 7.5 | 8.2 | — | 🟢 |
| ML 3 | 4.3 | 3.9 | 3.7 | 4.1 | 5.3 | 🟡 |
| ML 4 | 2.7 | 2.0 | 1.6 | 1.6 | 2.4 | 🔴 |
Safe depth for ≥6 mm TAD is reliably found only at ML 1 & ML 2.
Cortical Bone Thickness (CBT) – Mean values (mm)

| Level (ML) | Mean CBT (mm) | Range | Zone |
|---|---|---|---|
| ML 1 | 1.49 | 0.65–2.43 | 🟢 |
| ML 2 | 1.14 | 0.13–1.97 | 🟢 |
| ML 3 | 1.04 | 0.10–2.78 | 🟡 |
| ML 4 | 1.00 | 0.30–2.04 | 🟡/🔴 |
≥1 mm cortical thickness recommended for stability.
Quick Placement Guide
- 🟢 Best sites: Paramedian ML 1 & ML 2 (safe, accessible, adequate BD + CBT)
- 🟡 Variable sites: ML 3 (borderline, confirm with CBCT; angle placement if used)
- 🔴 Avoid: ML 4 (thin bone, risk of perforation, thick soft tissue, vessels nearby)
- ⚠️ Anterior caution: Stay clear of incisive canal (midline → only parasagittal placement)
- 💡 Trick: Angulated placement ↑ available BD in posterior palate
MCQs
- The most favorable default site for palatal miniscrew placement in adults is:
- A. Midline at incisive papilla
- B. Paramedian at premolar level (ML1–ML2)
- C. Paramedian at molar level (ML4)
- D. Far lateral palate near greater palatine foramen
Answer: B
Rationale: Anterior paramedian sites (premolar region) combine higher bone depth with thicker cortex and easier access, reducing perforation and stability risks.
- Which pattern best describes palatal bone depth (BD) across adults?
- A. Increases posteriorly and laterally
- B. Decreases posteriorly and laterally
- C. Constant across all levels
- D. Highest at molar level
Answer: B
Rationale: BD trends highest anteriorly near the midline and declines toward posterior and lateral regions.
- For reliable primary stability of orthodontic miniscrews, a practical cortical bone thickness (CBT) threshold is:
- A. ~0.3 mm
- B. ~0.7 mm
- C. ~1.0 mm or more
- D. >2.5 mm always required
Answer: C
Rationale: About 1.0 mm CBT supports favorable insertion torque and stability without excessive site trauma.
- To reduce perforation risk for a posterior paramedian placement without CBCT, the most sensible tactic is:
- A. Use longer screws (≥8 mm) and seat fully
- B. Perpendicular insertion with full seating
- C. Angulate insertion and/or accept partial seating
- D. Shift to the midsagittal plane
Answer: C
Rationale: Angulation increases traversed bone; partial seating reduces unintended nasal entry when BD is borderline.
- Regarding the incisive canal, safer placement strategy is:
- A. Sagittal midline at ML1
- B. Paramedian at ML1–ML2
- C. Midline further posterior
- D. Crossing incisive papilla intentionally
Answer: B
Rationale: Paramedian avoids nasopalatine canal while preserving favorable BD/CBT.
- A key anatomic hazard in the posterolateral palate is the:
- A. Lesser palatine artery
- B. Greater palatine neurovascular bundle
- C. Infraorbital nerve
- D. Nasopalatine nerve
Answer: B
Rationale: The greater palatine bundle courses posterolaterally and must be respected.
- During insertion, approaching the nasal floor is often signaled by:
- A. Sudden loss of torque
- B. Soft tissue blanching alone
- C. Firm “stop” from dense nasal cortical plate
- D. Immediate gingival bleeding
Answer: C
Rationale: The dense nasal cortex provides distinct tactile resistance with slow, controlled placement.
- Typical mean BD at ML4 (molar-level paramedian) is:
- A. >8 mm
- B. 5–6 mm
- C. 2–4 mm
- D. <1 mm
Answer: C
Rationale: Posterior paramedian BD is often shallow, making fully seated 6 mm screws risky.
- Adult left–right differences in palatal BD/CBT are generally:
- A. Large and significant
- B. Significant only in females
- C. Small and not statistically significant
- D. Left always greater than right
Answer: C
Rationale: Side differences are typically negligible compared to anterior–posterior patterns.
- Immediate loading feasibility most closely relates to:
- A. Soft tissue thickness
- B. CBT and insertion torque
- C. Screw head shape
- D. Chronologic age alone
Answer: B
Rationale: Cortical thickness drives insertion torque, which underpins primary stability for loading.
- A practical default screw length for anterior paramedian adult palate is:
- A. 4 mm
- B. 6 mm
- C. 10 mm
- D. 12 mm
Answer: B
Rationale: Around 6 mm balances safety and stability in typical anterior paramedian BD.
- Completely seating a 6 mm screw at ML4 commonly:
- A. Is always safe
- B. Risks nasal perforation
- C. Causes mucoceles routinely
- D. Increases CBT
Answer: B
Rationale: Shallow posterior BD increases perforation risk with full seating.
- Management of a small nasal perforation during palatal TAD placement generally involves:
- A. Mandatory surgical closure
- B. Immediate removal plus nasal packing in all cases
- C. Conservative observation; most heal uneventfully
- D. Systemic steroids
Answer: C
Rationale: Small perforations usually resolve; escalate only if symptomatic.
- The midsagittal suture is often excluded from generalized site recommendations because:
- A. CBCT artifacts dominate
- B. High anatomic variability across adults
- C. No cortical plate exists there
- D. It cannot be measured
Answer: B
Rationale: Suture variability undermines generalized midline guidance.
- The single strongest driver of miniscrew design/length selection is:
- A. Aesthetics
- B. Brand
- C. Placement site (location)
- D. Patient preference
Answer: C
Rationale: Local anatomy dictates diameter, length, and thread engagement strategy.
