🔎 Indications
- Supraerupted molars (commonly due to early loss of opposing tooth)
- Need for posterior intrusion to re-establish occlusion
- Minimally invasive alternative to surgery, headgear, or prosthetic crown reduction
🛠 TAD Design
- Material: Titanium alloy
- Size: 6–12 mm length, 1.2–2.0 mm diameter
- Fixation: Mechanical grip to cortical bone (not osseointegrated)
- Placement:
- Minimally invasive
- Often only topical anesthesia
- Inserted through gingiva into bone with hand driver
- Optional: mucosal punch/pilot hole in thick tissue or dense bone
- Loading: Immediate
- Removal: Simple hand unscrewing
- Failure rate: 9–30%
🔩 Types of TADs
1. Self-tapping
- Conical design, threaded shaft, tapered tip
- Requires pilot hole → then inserted with hand driver
2. Self-drilling
- Corkscrew design, threaded shaft, sharp tip
- Cuts through bone, expels debris
- Placed directly with hand driver (no pilot hole)
👩⚕️ Patient Selection
- ≥ 12 years (FDA approved)
- Avoid: growing patients (palatal suture), heavy smokers, bone metabolic disorders
Optimal Placement
- Maxilla:
- Between 2nd premolar & 1st molar (5–8 mm from alveolar crest)
- Angle: 30–45° to occlusal plane (posterior region)
- Palatal slope (avoid greater palatine nerve)
- Midpalatal region = D1/D2 bone
- Mandible:
- Either side of 1st molar (~11 mm from crest)
- Angle: 30–45° to occlusal plane
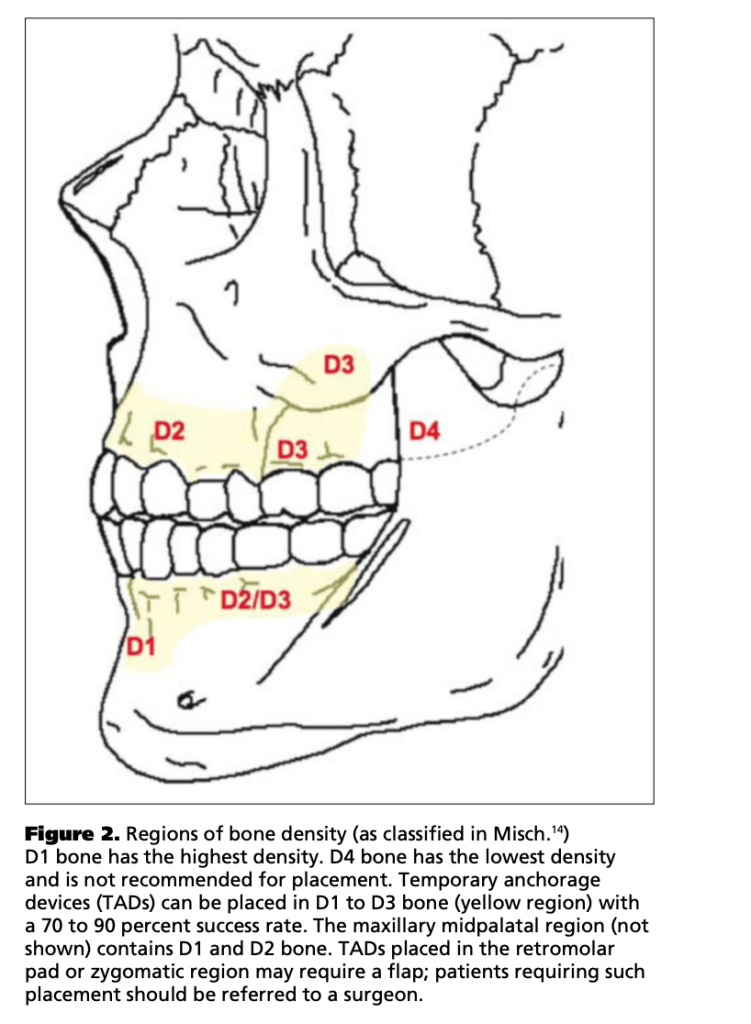
- Bone Density (Misch classification):
- Best: D1–D3 (dense cortical, anterior regions, palatal, posterior mandible)
- Avoid: D4 (tuberosity – failure rate up to 50%)
- Mnemonic: “One Oak, Two Pine, Three Balsa, Four Foam”
- Soft Tissue Health
- Better: Keratinized (attached) tissue → ↓ failure
- Worse: Nonkeratinized mucosa → gingival inflammation, overgrowth
- Tip: In buccal posterior, if risk of root proximity → place in alveolar mucosa
| Type | HU Range | Location | Analogy | TAD Suitability |
|---|---|---|---|---|
| D1 | >1250 HU | Anterior mandible, buccal shelf, midpalatal | Oak 🌳 | ✔ Best, may need pilot hole |
| D2 | 850–1250 HU | Ant. maxilla, midpalatal, post. mandible | Pine 🌲 | ✔ Good |
| D3 | 350–850 HU | Post. maxilla & mandible (thin cortex) | Balsa wood | ✔ Acceptable |
| D4 | 150–350 HU | Tuberosity region | Polystyrene foam | ❌ High failure (35–50%) |
Bone Availability (Safe Zones)
| Region | Best Site | Distance from Crest |
|---|---|---|
| Maxilla (posterior) | Between 2nd premolar & 1st molar | 5–8 mm |
| Mandible (posterior) | Either side of 1st molar | ~11 mm |
| Anterior (maxilla & mandible) | Between canine & lateral incisor | — |
If inadequate space:
- Palatal placement
- Root divergence before insertion
Insertion Technique
| Region | Angle of Insertion | Rationale |
|---|---|---|
| Posterior Maxilla | 30°–45° to occlusal plane | Cortical anchorage; balance safety & stability |
| Anterior Maxilla / Posterior Edentulous Maxilla | ~90° to occlusal plane (parallel to sinus floor) | Avoid sinus perforation, biomechanically better for molar intrusion |
| Mandible | 30°–45° to occlusal plane | Greater contact with thick cortical bone |
🔹 Tip: Orthodontic wire surgical stent may be used to guide accurate insertion

Force Loading Guidelines
| Condition | Recommended Force | Notes |
|---|---|---|
| General loading limit | ≤ 300 g | Beyond this = risk of failure |
| Thin cortical bone | ~50 g | (Dalstra) |
| Dense mandibular bone | Stable up to 900 g | (Buchter) |
| Maxillary molar intrusion (children) | 90 g | (Kalra) |
| Maxillary molar intrusion (adults) | 50 g | (Melsen) |
| Miniscrew-supported max molar intrusion | 100–200 g | Optimal range |
| En-masse intrusion (PM2 + M1 + M2) | 200–400 g/side | Requires more force |
| Miniplate-supported mand molar intrusion | 500 g | (Umemori) |
Post-Insertion Care
Chlorhexidine Rinse (0.12%)
- 10 mL BID for 1 week (continue if needed)
- Prevents soft tissue inflammation & overgrowth
- Slows epithelialization → keeps miniscrew head accessible
⚠️ Important Instruction for Patients:
- Wait 30 min after rinsing before brushing with fluoridated toothpaste (to avoid inactivation of chlorhexidine by anionic agents in toothpaste).
| Technique | Placement | Control of Tipping | Notes |
|---|---|---|---|
| Single TAD | Buccal dentoalveolus (between PM2 & M1 at mucogingival junction) | Transpalatal arch (TPA) with buccal root activation | TPA raised 3–5 mm → tongue pressure aids intrusion |
| Two TADs | Buccal: between M1 & M2 Palatal: slope between PM2 & M1 (medial to greater palatine nerve) | Elastic chain / NiTi coil passes diagonally across occlusal table | Risk of palatal tipping → may need partial braces |
| Palatal / Midline | Midline or palatal slope if interradicular space inadequate | Extension arm to reach slope; partial braces for control | Used when buccal bone insufficient |



Intrusion Rates
- Single M1 intrusion → 3–4 mm in ~6–8 months
- M2 intrusion → 1–2 mm in ~5 months
- En-masse PM2 + M1 + M2 → ~0.5 mm/month
Root Resorption Risks
- Mechanism: Intrusive force concentrates at apex → PDL compression → possible necrosis & resorption
- Evidence:
- Molars = second highest risk (after incisors)
- Documented in molars with:
- Tip-back mechanics
- High-pull headgear intrusion
- Distalization forces
- Range: 25–240 g can cause histologic resorption (Reitan)
- Controversy:
- Some studies show no significant difference between light (50 g) vs heavy (200 g) forces in resorption risk (Owman-Moll)
- Ari-Demirkaya et al. → Mean apical resorption only 0.18 ± 0.18 mm after 7 months
- Comparable to conventional orthodontics → not clinically significant
- Sinus floor effects:
- Intruding palatal root may lift sinus floor membrane intranasally
- Usually without complications
Risks & Complications
| Complication | Clinical Note | Management / Prognosis |
|---|---|---|
| Root trauma | Injury to PDL/root → possible vitality loss or ankylosis | If no pulp involvement → repair in 3–4 months |
| Anchorage failure | Miniscrews may loosen, tip, or extrude | Mobile screw → must be replaced; usually due to thin cortical bone or excessive force |
| Soft tissue irritation | More common in loose alveolar mucosa → inflammation, overgrowth, ulcers | Prefer keratinized tissue; hygiene + CHX rinse |
| Nerve injury | Greater palatine nerve risk in palatal slope (5–15 mm from gingival border, lateral to M2/M3) | Careful site selection & angulation |
| Sinus perforation | Small (<2 mm) usually self-heals, no effect on stability | Large perforation → possible sinusitis or oroantral fistula |
| Relapse | Extrusion of intruded molars common | Average relapse ≈ 30% |
