Anterior open bite is one of the trickiest malocclusions we deal with in orthodontics. It’s not just about teeth — skeletal, dental, functional, and even habitual factors play a role.
🔹 Traditional Approaches
For decades, open bites in adults were often corrected by:
- Extruding anterior teeth orthodontically (which works dentoalveolarly but doesn’t do much for facial esthetics in skeletal cases).
- Orthognathic surgery (Le Fort I osteotomy, sometimes two-jaw surgery) to reposition the maxilla.
These surgical approaches improve facial esthetics but come with a catch — relapse.
- Denison et al. found a 21% relapse at 1-year post-surgery.
- Proffit et al. reported 7–12% overbite reduction within 3 years after Le Fort I surgery.
🔹 The Game Changer: Skeletal Anchorage
With the introduction of absolute anchorage (miniscrews, miniplates), things got exciting. Now, orthodontists could correct open bites without surgery, by intruding the posterior teeth and letting the mandible autorotate upward and forward.
- Kuroda et al.: Skeletal anchorage makes open-bite treatment simpler than surgery.
- Sugawara et al.: Used miniplates to intrude mandibular molars; reported ~30% relapse after 1 year.
- Lee & Park: Miniscrew intrusion of maxillary molars → only 10.4% relapse in molars and 18.1% relapse in overbite at 1 year.
🛠️ How Was Intrusion Done?
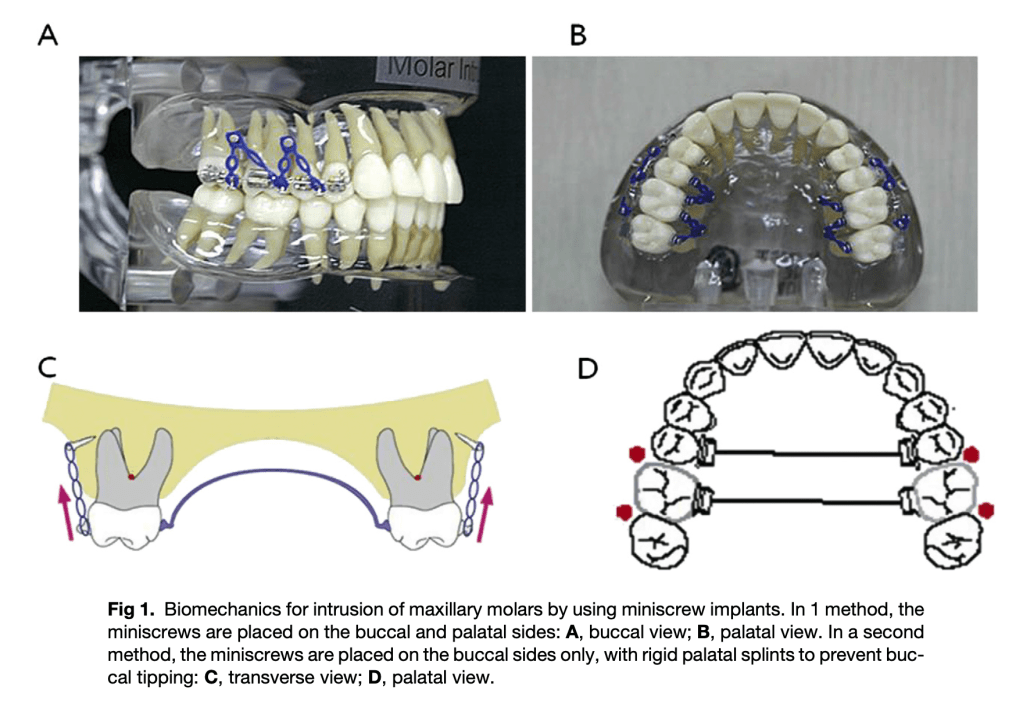
Two different miniscrew protocols were used:
1️⃣ Buccal + Palatal Screws
- Screws placed between roots of 2nd premolar–1st molar and 1st–2nd molar.
- Intrusive force applied with elastomeric chains after 1–2 weeks.
2️⃣ Buccal Screws Only
- Screws placed on buccal side at the same sites.
- Rigid transpalatal arch (TPA) added to prevent buccal tipping.
🔹 Maxillary vs. Mandibular Intrusion
- Umemori & Sugawara: Intruded mandibular molars → ~30% relapse in 1 year.
- Current study (Baek et al.): Intruded maxillary molars, since excessive eruption in that region often drives open bite
- ✅ Result: More fundamental correction compared to mandibular intrusion.
🔹 Measuring Stability Correctly
- Past studies measured incisal overlap directly, but this can be misleading when the mandible rotates during treatment.
- This study used new reference planes (HP & VP, based on SN line) to get more accurate and reproducible data.

🔹 Skeletal & Dental Changes Observed
- During treatment:
- Mandible rotated counterclockwise → bite closure.
- Pogonion moved forward & upward.
- Facial height decreased.
- Some anterior extrusion also helped deepen overbite.
- During retention:
- Relapse → molar eruption, clockwise rotation, pogonion downward/backward.
- BUT interestingly, maxillary incisors erupted slightly between year 1–3, which compensated for some relapse and deepened the bite again.
🔹 Relapse Pattern
- Most relapse (>80%) happened in the first year.
- After year 1, changes were minimal.
- Relapse mechanisms resembled orthognathic surgery relapse: molar eruption + mandibular clockwise rotation.
- Interpretation: It’s not just teeth—it’s also muscles & soft tissue adaptation trying to return to “old balance.”
🔹 Role of Retention & Soft Tissue
- Tongue posture, perioral muscles, and habits play a huge role.
- Myofunctional therapy after treatment improves stability.
- Standard retainers (lingual + circumferential) aren’t enough for intruded molars — because intrusion is inherently less stable than tipping or mesiodistal movement.
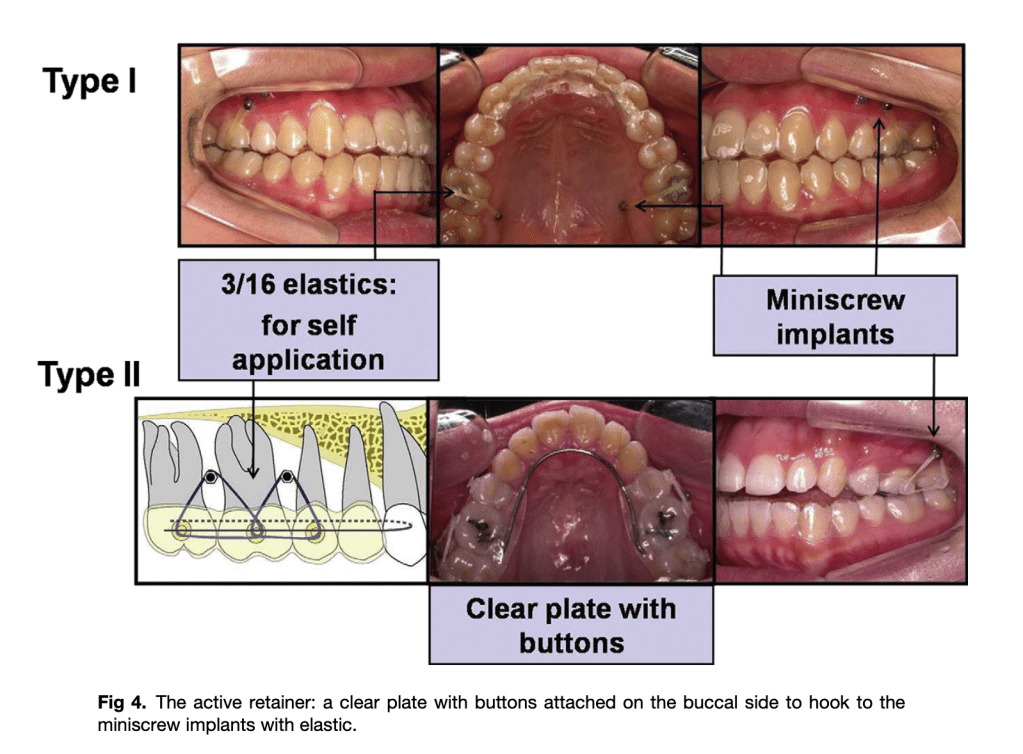
- Authors suggest an “active retainer”: clear retainer with buccal buttons that can be hooked to miniscrews with elastics to hold molars in place.