This “loose connective tissue” isn’t just chilling—it’s DIRECTING THE SHOW. Here’s the tea:
- Bone Resorption: Follicles send out signals like “Hey osteoclasts, wreck this bone!” to carve a path for the tooth. Think of it as a tiny demolition crew. 💥
- Deciduous Tooth Roots: They also dissolve baby teeth roots. RIP, milk teeth—you served us well. 🍼⚰️
- No Follicle? No Eruption. It’s like trying to launch a rocket without fuel. 🚀🙅♂️
Fun fact: If follicles throw a tantrum, you get eruption disturbances. Cue the ortho panic. 🆘
The Maxillary Canine: Ortho’s Problem Child 🦸♀️🦷
Ah, the upper canine—the Beyoncé of teeth (fierce, essential, but sometimes diva). When it decides to stay buried, you’ve got an impacted canine on your hands.
- Prevalence: 1-1.8% of people. More common in palatal positions (85%!). Ethnicity matters—some groups get hit harder. 🌍📊
- Gender Wars: Most studies say females > males, but Israeli data says it’s a tie. Canines don’t care about your gender norms. ✨⚧️
📌 Subject Selection: Not Random, But Relevant!
Before diving into imaging techniques, let’s address a key factor: selection bias.
📌 The kids in this study weren’t randomly picked—they were referred due to high risk of resorption from ectopic maxillary canines.
Does this affect the results? 🤔
➡️ Maybe, but not by much! The findings remain clinically relevant, though they might not be 100% applicable to a general school population.
🦷 Assessing the Dental Follicle: The Imaging Dilemma
So, how do we normally assess a follicle?
✔️ Clinical examination—Good for basics, but we need more.
✔️ Intraoral films—Useful, but might not show the full picture.
✔️ Conventional panoramic & full-mouth X-rays—Can sometimes fail at visualizing the true relationship between the ectopic canine and adjacent roots.
👉 Enter CBCT! This game-changer allows us to study the follicle in 3D, revealing its true shape, width, and relationship to other teeth.
⚠️ Radiation & Cost: Is CBCT Worth It?
CBCT is not all sunshine and rainbows. 🌦️ It comes with:
❌ Higher radiation exposure (2 to 8 times more than panoramic/conventional films).
❌ Increased cost.
But before you toss out your CBCT scanner, consider this:
✅ It provides a clearer, more accurate diagnosis, especially in high-risk resorption cases.
✅ The clinical benefits outweigh the risks, especially when determining treatment prognosis for ectopic canines.
📊 What Did CBCT Reveal About Follicle Width?
By analyzing scan by scan, we found:
✔️ Follicle width ranged from 0.5 mm to 7 mm.
✔️ Mean width: 2.9 mm (Confidence Interval: 2.7–3.2 mm).
✔️ Some follicles were 2 to 3 times wider than normal, indicating cystic transformation! 🦠
👉 In other words, big follicle = possible cystic changes, making CBCT invaluable for early intervention.
🦷 Cystic or Degenerative Changes in Dental Follicles
📌 Fact: During tooth eruption, dental follicles can undergo cystic or degenerative changes.
📌 Key Concern: Some wide follicles in this study had cystic degeneration, but they didn’t cause deviation in adjacent teeth—a usual warning sign.
👀 Why does this matter?
➡️ If a dental follicle undergoes cystic degeneration, it may turn into a dentigerous cyst—which is most common with maxillary canines.
🤔 Can We Reliably Detect Cystic Transformation?
🔍 Intraoral Films:
❌ Cannot reliably differentiate between a cyst and normal eruption-related changes.
🔍 CT Scans (Including CBCT):
❌ Even with CBCT, we still can’t reliably distinguish a physiologically enlarged follicle from one undergoing cystic transformation.
👆 Why? Because both might appear as enlarged follicles, and the distinction is only clear histologically.
👉 BUT WAIT! Do we always need to worry?
🛑 When Should We Be Concerned?
✅ Normally erupting canines? No big deal! As the tooth erupts, both the normal follicle and any cystic follicle will self-destruct when the crown reaches the gingiva. 🚀
✅ Ectopically positioned or embedded canines? ⚠️ These require monitoring during growth because they behave differently.
📌 Risk of Dentigerous Cysts in Impacted Teeth:
- 1 in 150 unerupted teeth may develop a dentigerous cyst (Mourshed & Toller).
- Risk increases after age 20, especially for impacted third molars.
📍 Canine Position & Follicle Width: What We Know
🔹 Buccally & Apically Displaced Canines 🟢
✅ Have wider follicles than normally positioned canines.
✅ More space → More follicle expansion!
🔹 Lingually Displaced Canines 🔵

🔹 Normally Positioned Canines 🟡
✅ Follicle width is about the same for both groups.
💡 What Does This Tell Us?
🦴 Hard tissue barriers—like adjacent incisor roots or a thick cortical bone layer (lingual to the alveolar process)—may restrict follicular expansion.
🦷 In contrast, thin cortical bone and spongeous bone allow the follicle to expand more freely.
📌 Key Takeaway: Follicle size is not random—it’s influenced by local bone density & space availability.
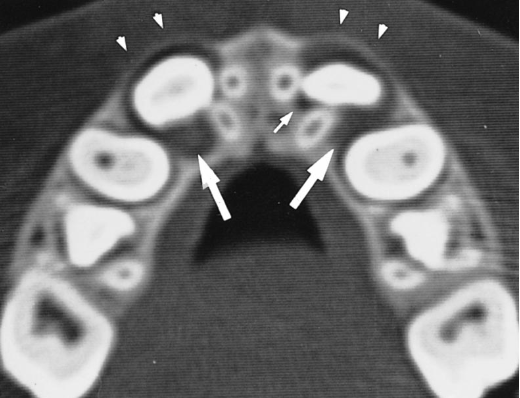
🔍 Follicle Shape & Jaw Bone Structure
📸 CBCT Scans Reveal an Interesting Pattern:
- 🟠 Loosely spongeous bone + spacious jaws → Follicle adapts a spherical shape 🔵
- 🔺 Limited space for expansion → Follicle takes on an irregular shape 🟠
🧐 Surprisingly, this hasn’t been reported before in literature!
🔬 Histological Findings (A.K.A. What’s Inside the Follicle?)
A total of 17 dental follicles underwent histological analysis, and here’s what was found:
✅ Loose connective tissue matrix—kind of like an unorganized dental construction site.
✅ Fragments of reduced enamel epithelium—because teeth love to shed layers.
✅ PMN cells (polymorphonuclear leukocytes)—a fancy way of saying “immune cells lurking around.”
✅ Microcysts or full cystic degeneration in 4 cases—a follicle’s way of saying, “I need space!”
⚠️ Do Enlarged Follicles Increase Root Resorption Risk?
👶 A Common Practice:
To prevent ectopic eruption, orthodontists often extract deciduous canines if the permanent canines have enlarged follicles.
Why?
🔹 Some believe widened follicles may:
1️⃣ Cause deviations in adjacent permanent roots.
2️⃣ Induce root resorption in neighboring incisors.
🔬 What This Study Says:
❌ No evidence confirms that widened dental follicles cause adjacent incisor root displacement.
❓ Root resorption risk remains unclear—this hasn’t been thoroughly investigated.
💡 Do Wide Follicles Push Teeth Around?
🔎 A common assumption is that large dental follicles could push adjacent teeth out of alignment.
📊 Reality Check: This study found that:
✅ Follicles expanded into spongeous bone → sometimes causing the alveolar cortex to bulge
✅ ❌ But they did NOT interfere with or deviate adjacent teeth!
👀 What actually caused root deviations?
➡️ Ectopically positioned canines exerting eruptive forces, NOT the follicles themselves!
📌 Do Sex, Age, or Eruption Stage Affect Follicle Size?
🟢 Nope! This study found NO significant relationships between:
- Follicle width & sex
- Follicle width & age
- Follicle width & canine eruption stage
🚀 Surprising Find:
No difference in follicle size was found between canines still in the bone crypt and those nearing eruption—unlike past radiographic studies. 📸
🔬 What Else Affects Follicle Size?
📊 Regression Analysis Says…
📉 The R² values suggest there are still unknown factors influencing follicle width. What could they be? 🤔
🔬 Likely Candidates:
1️⃣ Hormonal activity 🧬
2️⃣ Growth-related cellular changes ⚡
3️⃣ Innate genetic factors 🧪
📌 Key Takeaway:
Since canine eruption happens in bursts, follicle size may fluctuate over time rather than follow a steady pattern.
