Picture this: A young patient strolls into your ortho clinic with a large overjet, a long face, and a smile that shows more gum than teeth! 🦷😬 They’ve got highly visible incisors at rest, and when they grin, it’s all pink and no chill. As an orthodontist, you know this isn’t just about reducing that overjet—it’s a full-on battle for balance, aesthetics, and function. Welcome to the world of high-angle Class II div 1 patients! 💥
So, What’s the Game Plan? 🧐
You need to: ✔️ Reduce the overjet 🏹 ✔️ Control the visibility (and vulnerability) of those maxillary incisors 🦷 ✔️ Avoid unwanted movements that could make things worse! 🚫😵
Enter the hero of our story: The Removable Maxillary Appliance with Vertical Pull Headgear! 🎭 This setup is like giving your patient’s upper jaw a much-needed GPS system—guiding growth while keeping everything under control. 🚀
Why Headgear? 🎩
For our Class II, high-angle patients with a reduced or average overbite, regular distal movement of molars isn’t enough. The problem? If we let the molars extrude, we risk backward rotation of the mandible (a.k.a. making that long face even longer 😱). So, what’s the fix?
👉 High pull headgear! This keeps the maxillary molars in check, prevents unwanted rotation, and—bonus!—helps reduce that excessive gummy smile. 🎯
The Appliance Rundown 🦷
Now, you might be thinking, Why not just band the first molars and call it a day? Well, if only ortho were that easy! 🤷♂️
Attaching the headgear to molars alone can lead to: ❌ Buccolingual tipping (aka unstable tooth positioning) ⚖️ ❌ Poor tissue tolerance (ouch!) 😖 ❌ Limited effectiveness in controlling the entire dental arch 🏛️
That’s why orthopaedic force should be distributed across as much of the maxillary dental arch as possible! This is where removable appliances become our best friends. 🤝
What Does the Literature Say? 📚
The greats of ortho have weighed in on this battle: 🦷 Thurow (1975) introduced a maxillary splint for better vertical control. 🦷 Graber (1969), Joffe & Jacobson (1975), Fotis et al. (1984) all experimented with variations. 🦷 Caldwell et al. (1984) gave us more case studies showing successful results! 🏆
In short, headgear-supported removable appliances work, and they’re backed by years of research and success stories. 🚀
🎯 The Clinical Hypothesis: What Are We Trying to Fix?
The goal? To reduce maxillary incisor visibility and vulnerability by:
✅ Intruding the maxillary anterior teeth (because less gum, more aesthetic!)
✅ Controlling excessive maxillary downward growth
✅ Encouraging a slight forward rotation of the mandible (which helps reduce that overjet!)
Think of it like adjusting a camera angle for the perfect smile—no one wants an overexposed shot! 📸
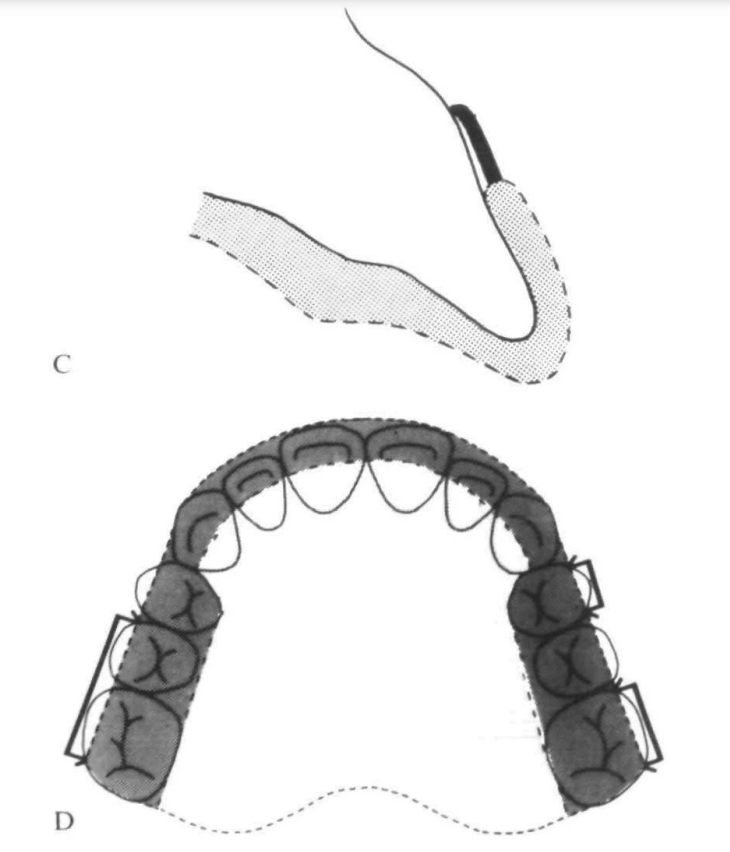
🛠️ The Appliance: M.I.S. Unpacked
So, what exactly is this M.I.S. (Maxillary Intrusion Splint)? 🤔
It’s a full-coverage, cribbed, heat-cured acrylic palatal plate (yes, that’s a mouthful—literally!). Here’s the breakdown:
🔹 Acrylic Capping: Covers the incisors and canines (only the incisal third) to provide stability.
🔹 Occlusal Coverage: Extends across the buccal segments but stops short of the buccal surfaces of premolars and molars (we don’t want to mess with transverse development).
🔹 Flying Extra-Oral Traction Tubes: Fancy name for where the headgear hooks in. These tubes are placed mesial to the first premolar cusp tip, allowing force application close to the maxillary dentition’s center of resistance (Poulton, 1959).
🔹 Anterior Clasp (Optional): A modified Southend clasp (basically a tiny goalpost 🏈 for your incisors) can be added to prevent palatal tipping.
Sounds cool, right? But wait—there’s more! 😆
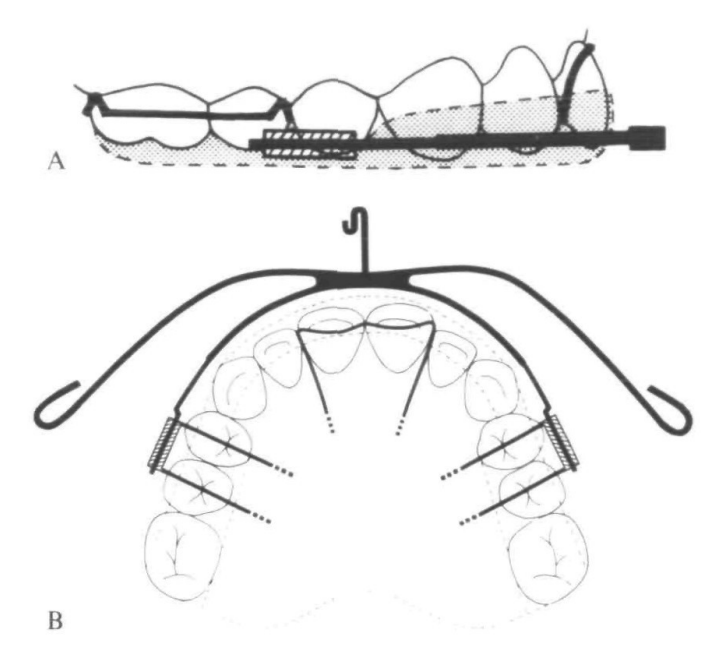
🦸♂️ The Heroic Headgear: Modified Lee Laboratory High-Pull Headgear
Now, headgear has a bit of a reputation (ask any patient who’s worn one… or any ortho student who’s explained one 🥲). But trust me, this isn’t your average high-pull headgear!
Here’s what makes it next level:
👉 Modified Elastic Traction Point: Instead of being in front of the ear, it’s shifted back behind the eye for a near-vertical force application. 🔼
👉 Angle of Pull: Around 60° to the occlusal plane—steeper than standard high-pull but way more effective for vertical control.
👉 Stiff Kloehn Bow: The 1.3mm inner arm provides better rigidity. (Because flimsy bows are not our vibe! 🙅♂️)
👉 Customized Outer Arm: Adjusted to deliver force through the center of resistance—ensuring movement is efficient, not chaotic.
And how much force are we talking about?
⚡ 500g or more bilaterally, depending on how much the patient can tolerate. (No pain, no gain? Well… maybe just a little discomfort! 😅)
⏳ Wearing Protocol: Commitment is Key!
Let’s be real—this isn’t a pop-it-in-once-a-day kind of appliance. Patients need to be:
🕒 Wearing it for up to 14 hours a day (yes, it’s bedtime bestie)
📈 Gradually introduced to the full wear schedule
🧠 Highly motivated (because compliance is everything!)
Treatment typically starts in the late mixed dentition phase, after:
✔ Preliminary expansion & arch rounding (about 3 months with a removable appliance)
✔ Maintaining arch coordination with a retainer when M.I.S. isn’t in use
For severe cases, we can add a mandibular traction plate for:
🔗 Class II intermaxillary elastics
🎯 Additional headgear reinforcement
(And yes, this setup makes the patient look like a sci-fi character, but hey—science is cool! 🤓)
🎯 Study Design: How Did We Test This?
We took 26 successfully treated Caucasian Class II Div 1 patients (11 males, 15 females) and compared them with 26 untreated patients waiting for treatment at Kingston Hospital (also 11 males, 15 females).
💡 Why? To compare how M.I.S. affects skeletal and dental parameters versus natural growth.
📊 Subject Data Summary (Mean Age ± SD)
| Group | Start of Active Treatment (X-ray 1) | End of Active Treatment (X-ray 2) |
|---|---|---|
| M.I.S. Group (n=26) | 11.4 ± 1.21 years | 12.5 ± 1.10 years |
| Control Group (n=26) | 11.0 ± 1.01 years | 12.7 ± 1.05 years |
👀 The control group had a longer observation period, so their data were adjusted using a computed factor (because growth doesn’t wait for anyone! ⏳).
🦴 Skeletal Changes: Shifting the Foundations
📍 Anteroposterior Changes
| Measurement | M.I.S. Group | Control Group | Significance (p-value) |
|---|---|---|---|
| SNA (°) (Maxillary prognathism reduction) | ↓ 1.18° | No change | P < 0.001 ✅ |
| N-A (mm) (Maxilla-to-nasion distance) | ↓ 1.21 mm | No change | P < 0.001 ✅ |
| S-ANS (mm) (Anterior nasal spine position change) | No increase | Increased by 1.29 mm | P < 0.001 ✅ |
💡 Translation: The M.I.S. helped keep the maxilla in check, while the control group’s maxilla kept growing forward like a rebellious teenager. 😎
📍 Vertical Skeletal Changes
| Measurement | M.I.S. Group | Control Group | Significance (p-value) |
|---|---|---|---|
| Mx-Md Plane Angle (°) | ↓ 1.04° | Smaller reduction | P < 0.01 ✅ |
| Sella-Nasion to Maxillary Plane (°) | Increased 0.90° | Smaller change | P < 0.01 ✅ |
💡 Translation: The M.I.S. helped tip the maxilla slightly backward, improving vertical control. Meanwhile, in the control group, nature did its own thing (and not in a good way). 😅
🦷 Dental Changes: The Real MVPs!
📍 Incisor and Overjet Adjustments
| Measurement | M.I.S. Group | Control Group | Significance (p-value) |
|---|---|---|---|
| Maxillary Incisor Proclination (°) | ↓ 10.98° | No major change | P < 0.001 ✅ |
| Overjet (mm) | ↓ 6.65 mm | No major change | P < 0.001 ✅ |
| Maxillary Incisor Intrusion (mm) | 1.50 mm | Extruded 0.42 mm | P < 0.001 ✅ |
💡 Translation: The M.I.S. successfully pushed the maxillary incisors up and back—a win-win for gummy smiles! 🎉 Meanwhile, the control group’s incisors just kept coming down like a curtain at a bad show. 😬

📍 Molar Changes: Moving the Big Players
| Measurement | M.I.S. Group | Control Group | Significance (p-value) |
|---|---|---|---|
| Maxillary Molar Distalization (mm) | 3.31 mm | Moved mesially 2.22 mm | P < 0.001 ✅ |
| Maxillary Molar Intrusion (mm) | 0.72 mm | Extruded 1.47 mm | P < 0.001 ✅ |
| Lower Molar Extrusion (mm) | 0.56 mm | No major change | P < 0.05 ✅ |
💡 Translation:
✔ M.I.S. pushed the upper molars back (goodbye Class II! 👋).
✔ The upper molars didn’t over-erupt, helping prevent an unwanted clockwise mandibular rotation (hello better profile!).
✔ The lower molars extruded slightly, helping maintain occlusal balance.
📢 What Did This Study Reveal?
This research confirmed that M.I.S. does the following efficiently:
✅ Reduces overjet & incisor proclination (Buh-bye, bunny teeth! 🐰)
✅ Distalizes first molars WITHOUT extrusion (A rare win! 🎉)
✅ Intrudes maxillary incisors effectively (No more gummy smiles! 👏)
✅ Prevents unwanted incisor extrusion (Unlike conventional mechanics)
✅ Maintains control over posterior facial height (No excessive vertical growth 😎)
💡 But wait… there’s a twist!
M.I.S. had little effect on forward mandibular growth, which was kinda disappointing. 😕 Some patients even had pogonion rotating backward (Oof! 🤦).
🦷 How Does M.I.S. Work?
It’s all about precision control:
🔹 Incisors move back & up → Less proclination, less overjet
🔹 Molars move back WITHOUT vertical elongation → No downward drift = No increased lower facial height
🔹 Slight maxillary restraint (sagittal & vertical) → No excessive maxillary growth
🔹 Mandibular changes? Meh. 😅
📊 Key Cephalometric Changes
| Measurement | M.I.S. Group | Control Group | Significance (p-value) |
|---|---|---|---|
| Overjet (mm) | ↓ 6.65 mm | No major change | P < 0.001 ✅ |
| Incisor Proclination (°) | ↓ 10.98° | No major change | P < 0.001 ✅ |
| Incisor Intrusion (mm) | 1.50 mm | Extruded 0.42 mm | P < 0.001 ✅ |
| Maxillary Molar Distalization (mm) | 3.31 mm | Moved mesially 2.22 mm | P < 0.001 ✅ |
| Maxillary Molar Intrusion (mm) | 0.72 mm | Extruded 1.47 mm | P < 0.001 ✅ |
💡 What does this mean?
- The incisors intruded and moved back, helping with overjet reduction.
- Molars moved back but didn’t drop down, keeping vertical dimensions in check.
- Mandible didn’t grow significantly forward, so this isn’t a cure for retrognathia.
🤔 So, Is M.I.S. a Miracle Appliance?
🎯 YES – For Mild to Moderate Class II Div 1 with a Gummy Smile!
🙅 NO – If You’re Expecting Major Mandibular Advancement!
👨⚕️ Key Takeaway for Ortho Students:
If you have a severely retrognathic mandible, M.I.S. alone won’t cut it. Combine it with a functional appliance (like a Herbst or Twin Block) for better mandibular effects!
🔍 Clinical Pearl: The ‘Pogonion Problem’
🧐 Some patients had pogonion rotating backward instead of forward!
🤷 Why? Those with a high FHMnP angle (steep mandibular plane) had less control over chin projection.
💡 Solution?
For these cases, consider:
✔ Intrusive activators to limit unwanted backward rotation
✔ Posterior bite blocks to control mandibular plane angle
📚 Previous Studies Agree! (We’re Not Making This Up! 😜)
🔹 Fotis et al. (1984) & Caldwell et al. (1984) → Molar intrusion leads to mandibular molar eruption as compensation.
🔹 Proffit (1986) → Better sagittal mandibular change when functional appliances + posterior bite blocks are used.
M.I.S. vs. Functional Appliances – Which One Wins? 🥊
🔹 M.I.S. (Maxillary Intrusion Splint) – The Gummy Smile Fixer
✔ Great for mild to moderate Class II Div 1 cases
✔ Reduces overjet, proclination, and gummy smile
✔ Intrudes incisors effectively without unwanted extrusion
✔ Works best when used in controlled cases
🚨 But… if the mandibular plane angle (FHMnP) is too steep, it won’t help much with mandibular growth! 😕
🔹 Functional Appliances (Bass, 1982 & Van Beek, 1982) – The Mandibular Booster
✔ Encourage forward mandibular growth
✔ Control vertical eruption of mandibular molars (posterior bite blocks FTW!)
✔ Work well for severely retrognathic patients
🚨 But… they don’t always intrude incisors as predictably as M.I.S.
🦷 Proffit’s Golden Rule (1986): Match the Appliance to the Case!
👨⚕️ Mild to Moderate Class II Div 1? → M.I.S. works great!
👨⚕️ Severe Retrognathia with High Mandibular Plane Angle? → Go for a functional appliance with posterior bite blocks!
📚 Clinical Pearl for Ortho Students!
🧐 Before choosing an appliance, always check:
✅ Mandibular plane angle (FHMnP) – Steep angles need bite block support!
✅ Severity of retrognathia – If severe, M.I.S. alone won’t do much!
✅ Vertical dimension changes – Don’t let mandibular molars erupt uncontrollably!
🚀 Moral of the Story: Ortho isn’t one-size-fits-all! Choose your tools wisely, and your patients will thank you. 🙌✨
🦷 Case History: Meet I.H. (The 9-Year-Old Who Got a Grown-Up Smile!)
📍 Initial Presentation
👦 9.4-year-old Caucasian male
😬 15 mm Overjet (Yikes!)
🦷 Spaced maxillary incisors with 3 mm midline diastema
😁 5 mm of incisor show at rest (a true gummy smile candidate! 👀)
Fun fact: He was NOT a digit sucker! (For once, we can’t blame thumbsucking! 😂)
📍 Treatment Plan
1️⃣ Phase 1:
- Upper removable appliance to expand buccal segments (arch coordination)
- Fixed appliance on 21|12 for closing anterior spacing
- Time: 4 months
2️⃣ Phase 2:
- M.I.S. + Intrusive Headgear + Mandibular Traction Plate
- Time: 20 months
3️⃣ Retention:
- Hawley Retainer (modified for mild forward mandibular posture)
- Worn nocturnally until late adolescence
📍 Final Result?
✅ Overjet gone!
✅ Gummy smile reduced!
✅ Class I occlusion achieved!
Moral of the case? The M.I.S. did its job perfectly! 🎯

🤓 Ortho Question Time! (Because Learning Should Be Fun! 🎉)
1️⃣ Would you use M.I.S. in your future patients? Why or why not? 🤔
2️⃣ What are your favorite patient excuses for not wearing their headgear? (Let’s laugh together! 😂)
3️⃣ If you had to invent a new orthodontic appliance, what would it do? (We love creative answers!) 🧠✨
Drop your answers in the comments below! 👇 Let’s geek out over ortho together! 🦷🎯
